
Observational Study
 Change in the Adiponectin and Metabolic Parameters After Metformin Treatment in Patients with Type 2 Diabetes Mellitus
Change in the Adiponectin and Metabolic Parameters After Metformin Treatment in Patients with Type 2 Diabetes Mellitus
1. Senior Resident, Department of Endocrinology, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India.
2. Assistant Professor, Department of Endocrinology, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India.
3. Associate Professor, Department of Endocrinology, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India.
4. Professor and Head, Department of Endocrinology, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India.
Abstract
Aim: To study the effect of metformin treatment on adiponectin levels and other parameters in newly diagnosed patients with type 2 diabetes mellitus.
Methods: This is a prospective observational study in a single centre where 46 patients with type 2 diabetes mellitus are included. Metformin is given to achieve the glucose control for 6 months and adiponectin levels are estimated at baseline and after 6 months of metformin treatment. The primary endpoint is to study the change in the adiponectin levels with metformin and secondary endpoint being change in the body mass index (BMI), fasting blood glucose (FBG), postprandial blood glucose (PPBG), haemoglobin A1c (HbA1c), lipid profile.
Results: BMI is reduced by 1 kg/m2 (p<0.0001), FBG and PPBG decreased from 155.2±27 mg/dL, 269±76.6 mg/dL at baseline to 102±16.7 mg/dL, 160±13.9 mg/dL after treatment (p<0.0001). HbA1c has decreased from 7.1±0.7% to 6.2±0.5% which is statistically significant (p=0.0001). In our study, total cholesterol (TC) and triglycerides (TG) has decreased from 203±3.5 mg/dL, 199.0 mg/dL from baseline to 189±33.0 mg/dL, 166±34.6 mg/dL after 6 months of metformin treatment respectively which is statistically significant (p=0.0001). LDL has decreased from 95.1±21.3 mg/dL to 94.0±17.8 mg/dL, but statistically not significant (p=0.359). The levels of high-density lipoproteins (HDL) have decreased from 39.1±4.7 mg/dL to 38.4±4.6 mg/dL which is also statistically not significant (p=0.240). There is significant increase in serum adiponectin level from 28.7±12.6 μg/mL at baseline to 36.4±12.5 μg/mL after 6 months of metformin treatment (p=0.0001). There is no correlation between adiponectin and BMI, BMI, FBG, PPBG, HbA1c and lipid profile. Mild gastrointestinal (GI) symptoms are seen in 4 patients. No patient reported hypoglycaemia.Conclusion: In conclusion, our study has shown the beneficial effect of metformin treatment on BMI, glycaemic control and improvement in the lipid parameters. There is significant elevation of adiponectin with metformin treatment but there is no correlation between adiponectin and the above parameters suggesting that these effects are through different mechanisms.
Keywords
Type 2 diabetes mellitus, metformin, BMI, adiponectin
Introduction
Type 2 diabetes mellitus (T2D) is characterized by insulin resistance and relative insulin deficiency. Adiponectin is secreted from the adipose tissue and implicated in insulin resistance and morbid obesity is associated with low levels of adiponectin.1-7Adiponectin secretion from subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) are also different.8Metformin is the first line drug in the treatment of T2D. Lot of mechanisms are proposed as the actions of metformin including activating mitogen activated protein kinase (MAPK) pathway and resultant reduction in the gluconeogenesis in the liver. It’s also proposed that metformin also acts through increasing adiponectin levels and consequent improvement in the insulin sensitivity.9 But the relation between metformin action and adiponectin levels is controversial as reported in the literature.10,11 So, we wanted to study the effect of metformin treatment on adiponectin levels and other parameters in newly diagnosed patients with T2D.
Patients and Methods
This is a prospective observational study done in the Department of Endocrinology, King George Hospital, Visakhapatnam, Andhra Pradesh, India from September 2018 to July 2019. Sixty-eight newly detected patients with type 2 diabetes mellitus and prediabetes attending the endocrinology OPD are included in the study. The American Diabetic Association (ADA) criteria are taken to define diabetes mellitus and prediabetes (diabetes mellitus when fasting plasma glucose is ≥126 mg/dL or post glucose plasma glucose ≥200 mg/dL, prediabetes when fasting plasma glucose is 100-125 mg/dL or post glucose plasma glucose 140-199 mg/dL). Patients who are controlled on diet and lifestyle measures are excluded from the study. Also, patients who required oral antihyperglycemic drugs (OAD) other than metformin and insulin are excluded. FBG, 2hr PPBG, HbA1c serum creatinine and lipid profile are estimated at baseline. These patients are started on metformin 1000 mg/day and dose adjusted to target diabetes control. The mean dose of metformin used is 740±350 mg/day (range 500-1500). Adiponectin levels are estimated at baseline and 6months after treatment. Adiponectin is measured by using RD191023100 human adiponectin enzyme-linked immunosorbent assay (ELISA), high sensitivity sandwich enzyme immunoassay (Biovender R&D products, Czech Republic). The lowest detectable range of adiponectin is 5 μg/mL.
Statistical analysisStatistical analysis is done using SPSS software version 16. Pearson correlation analysis is used to determine the strength of association between parameters. R value of 0.8 to 1.0 is considered significant.
Results
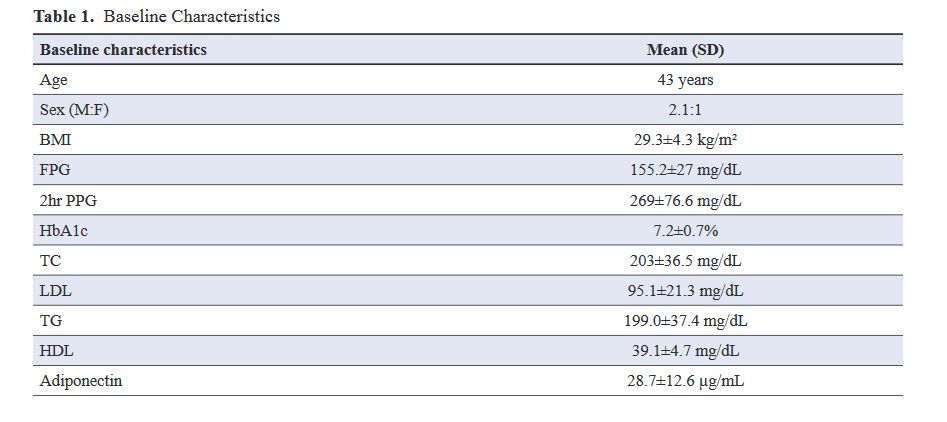
Out of total 64 patients, 10 patients required other OADs and insulin whereas 5 controlled on only lifestyle measures and medical nutrition therapy. Three patients didn’t turn up for the follow up. So, the final analysis is done in 46 patients with type 2 diabetes mellitus. Baseline characteristics are depicted in Table 1. The mean age of the patients is 43 years in our study and maximum number are between 40 to 60 years. Males are more than females in our study. The mean FPG is 155.2±27 mg/dL and 2hr PPG is 269±76.6 mg/dL with HbA1c of 7.2±0.7%. Baseline lipid parameters include total cholesterol 203±3.5 mg/dL, low-density lipoproteins (LDL) cholesterol 95.1±21.3 mg/dL, triglycerides 199±37.4 mg/dL and mean HDL 39.1±4.7 mg/dL. The mean adiponectin in our study is 28.7±12.6 μg/mL.
After metformin treatment:
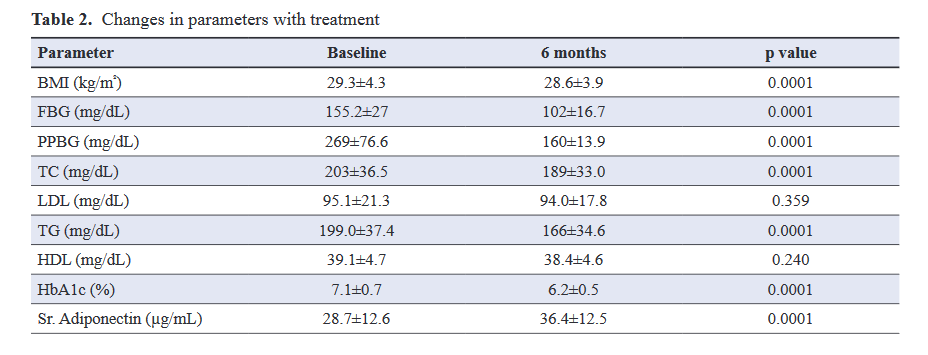
The results are depicted in Table 2.
6 months after metformin treatment, BMI has significantly decreased from 29.3±4.3 kg/m2 to 28.3±3.9 kg/m2. FBG and PPBG decreased from 155.2±27 mg/dL, 269±76.6 mg/dL at baseline to 102±16.7 mg/l, 160±13.9 mg/dL after treatment both are statistically significant (p<0.0001). HbA1c has decreased from 7.1±0.7% to 6.2±0.5% which is statistically significant (p<0.0001). In our study, TC and TG has decreased from 6.2±0.5% mg/dL, 199.0 mg/dL from baseline to 189±33.0 mg/dL, 166±34.6 mg/dL after 6 months of metformin treatment respectively which is statistically significant (p=0.0001). LDL has decreased from 95.1±21.3 mg/dL to 94.0±17.8 mg/dL, but statistically not significant (p=0.359). The levels of HDL have decreased from 39.1±4.7 mg/dL to 38.4±4.6 mg/dL which is also statistically not significant (p=0.240). There is significant increase in serum adiponectin level from 28.9±12.4 μg/mL at baseline to 36.4±12.5 μg/mL after 6 months of metformin treatment (p<0.0001). There is no correlation between adiponectin and BMI, FBG, PPBG, HbA1c and lipid profile. Four patients had mild GI symptoms and none had hypoglycaemia.
Discussion
This is a single centre prospective observational study from a tertiary care hospital from south India. Most of the patients are in the age group of 40 to 60 years which confirms with the known fact that incidence of diabetes mellitus increases with age. Around 40% are obese and 14% are overweight in our group which predisposes to T2D. The mean adiponectin levels are 28.7±12.6 μg/mL. The mean dose of metformin used in our patients is 740±350 mg/day (range 500-1500). BMI decreased by 0.7% (29.3±4.3 to 28.6±3.9 kg/m2). In most of the studies, it was shown that metformin is weight neutral. The weight reduction in our study could be influenced by both lifestyle intervention and dietary modification. In some of the studies, it was shown that metformin itself can reduce weight. The proposed mechanisms are by reducing the appetite, by increasing the utilization of more glucose in the GI epithelial cells and also through increasing the GLP-1 secretion. There is significant reduction of both fasting and postprandial blood glucose. HbA1c is reduced by 0.9% (7.1-6.2%) with metformin treatment which is observed in other studies also. In our study, there is a favourable effect of metformin on lipid profile. There is reduction in both total cholesterol and triglycerides after metformin treatment though we cannot totally exclude the effect of lifestyle intervention and glucose lowering on lipids.
The primary objective of our study is to look for the effect of metformin on serum adiponectin levels. There is significant improvement in adiponectin levels with metformin (28.7±12.6 to 36.4±12.5 μg/mL). In a meta-analysis by Su et al., Similar improvement with metformin was observed.12 In another study by Zulian A et al., metformin treatment resulted in increase in the expression and secretion of adiponectin in SAT but not in VAT in vitro.13 They also observed increase in adiponectin and reduction in the macrophage activation marker i.e., cluster of differentiation 68 (CD68) only in SAT and not in VAT even in the in vivo experiment suggesting that metformin alters adiponectin by modifying the adipose tissue inflammation. Whether metformin directly acts over the adipose tissue through MAP kinase pathway or alters adipogenes and increases the adiponectin or is it surrogate effect of appetite and glucose reduction or effect of altered lipolysis and lipogenesis, is not known.
There is no correlation between BMI and adiponectin in our study though there is weight reduction and increase in the adiponectin levels observed, in our patients six months after metformin therapy. BMI assesses both visceral and subcutaneous adipose tissue whereas the contribution of these two portions of fat tissue to the serum adiponectin levels is controversial. Kovacova Z et al.. studied the effect of obesity on adiponectin and found that the secretion of total adiponectin is less in the adipose tissue explants from subcutaneous adipose tissue (SAT) and not in visceral adipose tissue (VAT) in obese individuals.14 Nonobese people secreted more amount of high molecular weight (HMW) adiponectin from VAT whereas this difference is not seen in obese people. So various monomers of adiponectin may be more relevant in obese and nonobese individuals. After bariatric surgery induced weight loss, it was found that HMW adiponectin levels increased with weight loss.15 So different monomeric forms estimation may be more appropriate than measuring total adiponectin levels. In our study, glucose lowering is not associated with the increase in adiponectin levels. Blood glucose control by metformin is by reducing the gluconeogenesis from the liver whereas increment in adiponectin may be by the independent action of metformin on adipose tissue and that will explain the noncorrelation between glycaemic control and increment in the adiponectin. Mercedes et al.showed that adiponectin alters insulin sensitivity and low adiponectin levels are associated with reduced fatty acid oxidation in the muscle increasing the insulin resistance.16 It was also explained that metformin improves insulin sensitivity and adiponectin may be a marker of insulin sensitivity. But there can be other reasons for change in the adiponectin values like role of exercise, inflammation, ratio of subcutaneous to visceral adiposity. Our study didn’t show any correlation between adiponectin and various lipid parameters. Again, this finding suggests that the beneficial effect of metformin on lipid parameters are through multiple mechanisms and adiponectin may or may not be responsible for this effect.
Limitations
The sample size is small and proportion of visceral and subcutaneous adipose tissue is not measured. Insulin resistance is also not estimated.
Summary
In conclusion, our study has shown the beneficial effect of metformin treatment on BMI, glycaemic control and improvement in the lipid parameters. There is significant elevation of adiponectin with metformin treatment but there is no correlation between adiponectin and the above parameters suggesting that these effects are through different mechanisms.
Declaration of conflicting interest
The authors declare no conflict of interest pertaining to this study.
Funding
No funds are received for the conduct of study from any agency. The hospital being government owned, everything is free and adiponectin was purchased from personal funds.
Ethical Approval
Since this study is an observational study, there is no need of ethics committee approval.Approval was obtained from the super speciality board committee.
References
1. Liu C, Feng X, Li Q, Wang Y, Li Q, Hua M. Adiponectin, TNF-α and inflammatory cytokines and risk of type 2 diabetes: A systematic review and meta-analysis. Cytokine. 2016; 86:100-109.
2. Galic S, Oakhill JS, Steinberg GR. Adipose Tissue as an Endocrine Organ. Mol Cell Endocrinol. 2010 25;316(2):129-39.
3. Balsan GA, Vieira JLDC, de Oliveira AM, Portal VL. Relationship between adiponectin, obesity and insulin resistance. Rev Assoc Med Bras (1992). 2015; 61(1):72-80.
4. Flier EL. Obesity. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A eds. Williams textbook of endocrinology 14th edition. Elsevier; 2019:1573.
5. Pajvani UB, Scherer PE. Adiponectin: Systemic Contributor to Insulin Sensitivity. Curr Diab Rep. 2003; 3(3):207-13.
6. Guenther M, James R, Marks J, Zhao S, Szabo A, Kidambi S. Adiposity distribution influences circulating adiponectin levels. Transl Res. 2014; 164(4):270-277.
7. Kopp HP, Krzyzanowska K, Möhlig M, Spranger J, Pfeiffer AFH, Schernthaner G. Effects of Marked Weight Loss on Plasma Levels of Adiponectin, Markers of Chronic Subclinical Inflammation and Insulin Resistance in Morbidly Obese Women. Int J Obes (Lond). 2005; 29(7):766-71.
8. Reneau J, Goldblatt M, Gould J, Kindel T, Kastenmeier A, Higgins R, et al. Effect of adiposity on tissue-specific adiponectin secretion. PLoS ONE 2018; 13(6):e0198889.
9. Ahima RS. Adipose Tissue as an Endocrine Organ. Obesity (Silver Spring). 2006; 14 Suppl 5:242S-249S.
10. Abdelgadir M, Karlsson AF, Berglund L, Berne C. Low serum adiponectin concentrations are associated with insulin sensitivity independent of obesity in Sudanese subjects with type 2 diabetes mellitus. Diabetol Metab Syndr. 2013; 5:15.
11. Snehalatha C, Yamuna A, Ramachandran A. Plasma Adiponectin Does Not Correlate With Insulin Resistance and Cardiometa-bolic Variables in Nondiabetic Asian Indian Teenagers. Diabetes Care. 2008; 31(12):2374-2379.
12. J-R Su , Z-H Lu , Y Su , N Zhao , C-L Dong , L Sun, et al. Relationship of Serum Adiponectin Levels and Metformin Therapy in Patients With Type 2 Diabetes. Horm Metab Res. 2016; 48(2):92-8.
13. Zulian A, Cancello R, Girola A, Gilardini L, Alberti L, Croci M, et al. In Vitro and in Vivo Effects of Metformin on Human Adipose Tissue Adiponectin. Obes Facts. 2011; 4(1):27-33.
14. Z Kovacova , M Tencerova, B Roussel, Z Wedellova, L Rossmeislova, D Langin, et al. The Impact of Obesity on Secretion of Adiponectin Multimeric Isoforms Differs in Visceral and Subcutaneous Adipose Tissue. Int J Obes (Lond). 2012; 36(10):1360-365.
15. Auguet T, Terra X, Hernández M, Sabench F, Porras JA, Orellana-Gavaldà JM, et al. Clinical and Adipocytokine Changes After Bariatric Surgery in Morbidly Obese Women. Obesity (Silver Spring). 2014; 22(1):188-94.
16. Gil-Campos M, Cañete RR, Gil A. Adiponectin, the Missing Link in Insulin Resistance and Obesity. Clin Nutr. 2004; 23(5):963-74.
