
Review
 Management Strategies to Lower Risk of Atherosclerotic Cardiovascular Disease (ASCVD) in High-Risk South Asians
Management Strategies to Lower Risk of Atherosclerotic Cardiovascular Disease (ASCVD) in High-Risk South Asians
Senior Diabetologist, Advance Diabetes and Critical Care, Holy Help Hospital, Hisar, Harayana, India.
Abstract
The review focuses on South Asians (SA) with lipoprotein abnormalities and addresses risk stratification and management strategies to lower atherosclerotic cardiovascular disease (ASCVD) in this high-risk population. SAs have lower low-density lipoprotein cholesterol (LDL-C) compared with Whites and at any given LDL-C level, higher risk of myocardial infarction (MI) and coronary artery disease (CAD) are seen in SA ethnicity when compared with other non-Asian groups. SAs have higher triglycerides and lower high-density lipoprotein cholesterol (HDL-C) with smaller particle sizes of HDL-C compared with Whites, which strongly indicates high prevalence of metabolic syndrome in SAs. Compared with other ethnic groups SAs have higher lipoprotein (a) (Lp(a)) levels and this unique Lp(a) profile plays a vital role in the elevated risk of ASCVD in SAs. Studies which evaluate dietary patterns of SAs in the U.S show high consumption of carbohydrates and saturated fats. SA ethnicity has a high-risk lipoprotein profile and multifactorial lipid abnormalities play a central role in the pathogenesis of CAD. To understand the impact of the various lipoproteins and their contribution to increasing ASCVD in SAs more studies are desired. In high-risk groups aggressive lowering of LDL-C by using lifestyle modification including dietary changes and medications, such as statins, are essential in overall CAD risk reduction.
Keywords
Lipids, South Asians, dyslipidaemia, low-density lipoprotein, high-density lipoprotein
Introduction
South Asians (SAs), individuals who originate from countries including India, Pakistan, Nepal, Bangladesh, Sri Lanka, and Bhutan, comprise approximately 1.8 billion or one-quarter of the world’s population.1-4 Higher ASCVD risk in SAs may be explained, in part, by a higher prevalence of traditional risk factors such as diabetes, dyslipidaemia, hypertension, obesity, and tobacco use.5,6 Additionally, SAs experience premature coronary artery disease (CAD) with 3–5-fold higher risk of morbidity and mortality from heart disease as compared with individuals from other countries.6-9 SAs are a heterogeneous population arising from various religions and racial and cultural backgrounds; however, they share several characteristics. 10-14
In the Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction (INTERHEART) case-control study of 14,820 individuals from 52 countries that included acute myocardial infarction (AMI) cases and controls from 5 different SA countries, it showed an association between hypertension, diabetes, smoking, waist/hip ratio, diet, physical activity, and apolipoprotein levels with AMI among all populations including SAs.15 The risk factors associated with the highest population attributable risk among SAs were elevated Apo B100/Apo A-I ratio (46.8%), waist to hip ratio (37.7%), and smoking (37.5%).5,6,15 Dyslipidaemia was found to have the strongest association with AMI in SAs, indicating that it is vital in understanding the pathogenesis and evolution of ASCVD in SAs. Kalhan et al. demonstrated that SAs that migrate to the U.S have an adverse metabolic profile with an abnormal plasma lipid profile, higher plasma insulin levels, and truncal skin-fold thickness in their young adulthood compared with their European counterparts.16 In addition, the SHARE study evaluated disease risk factors and its relationship to subclinical atherosclerosis in 985 participants of SA, European, and Chinese descent residing in Canada. SAs were found to have higher total cholesterol, low-density lipoprotein cholesterol (LDL-C), triglycerides, and lipoprotein (a) (Lp(a)) levels, as well as increased prevalence of glucose intolerance and other risk factors compared with Europeans and Chinese. 17,18
Dyslipidaemia
Total Cholesterol, LDL-C, and VLDL-C
Elevated cholesterol, particularly LDL-C, is a well-established risk factor for coronary artery disease (CAD) and a target for therapy to decrease ASCVD risk. Elevated LDL-C is also a risk factor for CAD in SAs with risk of AMI increasing with rising LDL-C levels.19 Karthikeyen et al. demonstrated a large variation in LDL-C levels among different Asian subgroups in the INTERHEART study. SAs had lower mean LDL-C levels compared with people from Southeast Asia (Singapore, Malaysia, Thailand, and the Philippines) and Japan (LDL-C 125 mg/dL compared with 150 mg/dL in Southeast Asians and 134 mg/dL in Japanese).15
Moreover, for a given LDL-C level, the risk of MI and CAD is higher among SAs compared with other groups.15,20,21 This indicates that SAs have a high risk of AMI even at normal to low LDL-C levels. This heightened risk among SAs is likely secondary to smaller LDL particle sizes that are denser and therefore more atherogenic.22 In a study by Kulkarni et al.,the prevalence of small dense LDL (sdLDL) particles was higher in Asian Indians compared with Whites (44% versus 21%; p< 0.05).23 SAs with high levels of small dense LDL particles also have high fasting insulin levels, further suggesting that insulin resistance may be playing an important role in the increased prevalence of small, dense LDL particles.23,24 Overall, data suggest that smaller, denser LDL particles and higher concentrations of apolipoprotein B (ApoB) may be the driving factor in the elevated risk of CAD even at lower LDL-C concentrations.
HDL-C
High-density lipoprotein cholesterol (HDL-C) concentrations are generally inversely associated with ASCVD.25 Compared with other ethnic groups, SAs tend to have lower HDL-C and apolipoprotein A (ApoA) levels.2,15,26 However in SAs, HDL particles may be dysfunctional with pro-inflammatory and pro-oxidant effects, therefore contribute to increased ASCVD risk.27,28 In a small cross-sectional study by Dodani et al., 50% of the participants had dysfunctional HDL particles with HDL inflammatory index of ≥1.0, and dysfunctional HDL-C was significantly correlated with higher intimal medial thickness in the common carotid artery (CCA-IMT).29
This pattern of low HDL-C levels and dysfunctional HDL particles has been linked to insulin resistance and the increased prevalence of multiple sclerosis (MS) in SAs.30,31 In a study that evaluated MS and its association with HDL function, APOA1 gene polymorphisms and subclinical CAD, there was an association between MS and ApoA1 levels as well as APOA2 polymorphisms. The researchers postulated that this could lead to dysfunctional and low HDL in SAs predisposing them to an increased ASCVD risk.32
SAs tend to have HDL particles that are smaller in size, which could also be contributing to the abnormal function of HDL. Superko et al. studied metabolic disorders linked to CAD in Asian Indian men compared with age-matched men not of Indian descent; the Asian Indian group had a higher prevalence of low HDL2b (p<0.0002), even among the subgroup with HDL-C >40 mg/dL.33 They suggested that this could explain impaired reverse cholesterol transport in SAs. In a study comparing concentrations of large and small HDLC in Asian Indian men to white men in the Framingham Offspring Study, the Asian Indian men had higher concentrations of small HDL-C, lower concentrations of large HDL-C, and smaller particle size compared with Whites.30
Triglycerides
SAs tend to have a higher prevalence of hypertriglyceridemia. In a study by Misra et al., SAs had higher plasma triglycerides than Whites, with dyslipidaemia occurring at lower levels of BMI in SAs.34,35 Another comparative study revealed that Asian Indians in the Unites States compared with Whites have 2-fold higher hepatic triglyceride content (1.94 vs. 0.75%, respectively; p<0.001.36 SAs may be predisposed to increased levels of ectopic fat (deposition of triglycerides in non-adipose tissue such as the liver and muscle) that disrupts glucose-insulin metabolism resulting in MS and insulin resistance that contribute to elevated triglycerides. Shah et al. found higher hepatic fat, intermuscular fat, and visceral fat in SAs compared with other ethnicities (Whites, African Americans, Chinese Americans and Latinos).37 SAs also have a less favourable adipokine profile which could potentially play a vital role in their predisposition to cardiometabolic disease.37 In a study evaluating dyslipidaemia patterns in various races, Asian Indians had a higher risk of having combined dyslipidaemia which included high triglycerides. They were found to be twice as likely to have higher triglycerides compared with Whites (55.3% vs. 42.5%) with OR 2.12 for women and 2.67 for men; p<0.001.38
Cholesteryl ester transfer protein (CETP) is a plasma protein that mediates the transfer of triglycerides from triglyceride-rich lipoproteins to HDL and LDL particles in exchange for cholesteryl esters resulting in low HDL-C and small dense LDL.39Abnormalities in CETP are linked to accelerated atherosclerosis. SAs have higher CETP activity compared with Whites and this in turn is positively associated with higher triglycerides and LDL-C, but inversely related to HDL-C.40
Lp(a)
Elevated Lp(a) levels are an independent risk factor for ASCVD.41-44 Some but not all studies have shown that SAs have high Lp(a) levels.45,46 Palaniappan et al. compared 210 women <30 years old from three different ethnic groups (Whites, African Americans, and Asian Indians) in the United States. Asian Indian women had higher Lp(a) levels than Whites but lower than African American women (0.3 g/L in SAs, 0.5 g/L in African Americans, and 0.2 g/L in Whites, p<0.0001).47
There are some data to suggest that there is an association between Lp(a) and atherosclerosis in SAs. In a study looking at the association between Lp(a) and subclinical atherosclerosis by measuring CCA-IMT in diabetic South Indians, Lp(a) levels had a strong association with CCA-IMT.48 In another study that evaluated Lp(a) levels in young north Indian patients with MI, the mean Lp(a) was 22.3±5.4 mg/dL in MI patients compared with 9.3±22.6 mg/dL in the healthy control group.49 In the INTERHEART study, Lp(a) levels and risk of MI were studied among seven ethnic groups. Higher Lp(a) concentrations were associated with an increased risk of MI and a high population burden was noted in SAs with the population attributable risk of high Lp(a) for MI to be 9.5% in SAs compared with 0% in Africans.50
The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study was a prospective observational cohort study of 906 SA men and women aged 40–84 years living in the U.S, designed to study cardiovascular risk factors and subclinical CVD.51,52 In the MASALA, Lp(a) had no association with subclinical atherosclerosis including coronary artery calcium (CAC) (p=0.98), internal carotid IMT (ICA-IMT) (p=0.46), and CCA-IMT (p=0.97).53 Additionally, Lp(a) had no association with progression or incidence of CAC in the MASALA.4
Management of Dyslipidaemia
Risk Assessment Tools
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) ASCVD risk assessment guidelines included the Pooled Cohort Equations (PCE) to estimate the 10-year risk by race/ethnicity (Whites or African American) and sex for the first ASCVD event. For other ethnicities including SAs, the guidelines suggest using the equation for Whites and SA ancestry is now included as a “risk-enhancing factor” in the new cholesterol guidelines; therefore, after calculation of PCE, this risk-enhancing factor may favour initiation of statin or if already on statin intensification of therapy. 54
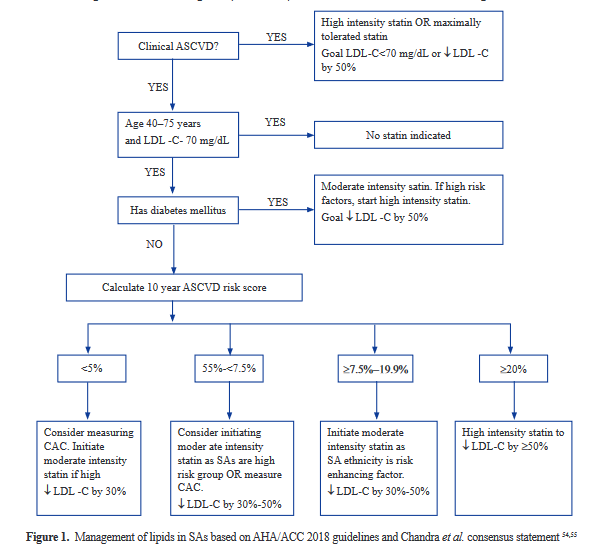
Use of StatinsA consensus statement on dyslipidaemia management in SAs was published by Chandra et al.55 According to this statement, statins are the mainstay in treatment of dyslipidaemia in SAs to lower LDL-C with a goal of LDL-C <100 mg/dL in high-risk and LDL <70 mg/dL in very high-risk patients.
A study by Gupta et al. evaluated statin effects on LDL-C and HDL-C in SAs and whites.56 They found one large trial that included SAs was the Heart Outcomes Prevention Evaluation-3 (HOPE-3) trial, with India being one of the participating countries. HOPE-3, a primary prevention trial looking at patients with intermediate risk, demonstrated that treatment with rosuvastatin 10 mg daily resulted in a significantly lower risk of cardiovascular events than placebo.57 A small study looking at pharmacokinetics and pharmacogenetics of statins in Asian Indians compared with Whites revealed higher peak plasma concentrations in Asian Indians, indicating possible increased risk of side effects at higher doses of statins in SAs.58 The SLCO1B1 C allele is a risk factor for statin-induced myopathy by causing lower statin uptake by the liver. A study done in Kerala, a region of southern India, revealed the presence of this variant in 15% of the population further postulating increased propensity for statin-induced myopathy in certain groups of SAs.59,60
Based on the current guidelines, it is reasonable to treat SAs on maximally tolerated statins like other ethnic groups while closely monitoring for side effects. Management strategies for dyslipidaemia in SAs are largely based on the new guidelines published by AHA/ACC and other societies in 2018(Figure 1).54
In SAs aged 40–75 years without diabetes mellitus who have LDL-C >70 mg/dL and intermediate risk (7.5%–19.9%), initiate moderate intensity statin therapy and consider initiating statin therapy for those at borderline (5.0%–7.5%) risk, as being SA is a risk-enhancing factor.
If risk-based decisions remain uncertain, among the intermediate risk group with an ASCVD score ≥7.5%–19.9% or among select borderline risk (5.0%-7.5%), it is reasonable to measure CAC to guide decisions to start a statin.
In SAs with severe hypercholesteremia (LDL-C ≥190 mg/dL) start high-intensity statin—no need to calculate the ASCVD risk score.
Since being SA is a risk-enhancing factor, if risk <5%, we recommend consideration of measuring CAC.
Combination Drug Therapy
Addition of Ezetimibe
Ezetimibe is a non-statin medication used to treat hyperlipidaemia. It is an inhibitor of intestinal cholesterol absorption and reduces total cholesterol, LDL-C, apolipoprotein B, and non-HDL-C. Ezetimibe lowers LDL-C by inhibiting the activity of Niemann-Pick C1-like 1 (NPC1L1) protein.61
The Intensive Versus Standard Blood Pressure Lowering to Prevent Functional Decline in Older People (INFINITY) study, comprising SA Canadians assessed the effectiveness of ezetimibe in patients with CAD or diabetes who were already on statin therapy in a randomized trial.62 At 6 weeks, patients that took ezetimibe plus statin were more likely to achieve goal LDL-C <77 mg/dL compared with the statin doubling group (68% vs. 36%; p=0.03) with an OR (95% CI) of 4.0 (1.2, 13.2). At 12 weeks, 76% of ezetimibe plus statin patients achieved target LDL-C compared to 48% (p=0.047) of the statin doubling group (adjusted OR (95% CI)=3.31 (1.01, 10.89)). The ezetimibe plus statin was generally well tolerated.62 The 2018 AHA/ACC guidelines stated that in patients who are very-high risk, we should aim to reduce LDL-C by 50% and that an LDLC threshold ≥70 mg/dL despite maximally tolerated statin would favour the additional initiation ezetimibe as a second-line agent.54
Role of FibratesFibrates increase HDL-C, lower triglycerides, and increase the LDL particle size. This pattern can potentially benefit SAs as they are prone to higher triglycerides, dysfunctional HDL, and smaller LDL particles. There are no clinical outcome trials in SAs looking at effects of fibrates. There were two large studies in the U.S which evaluated whether fibrates reduce CVD risk in diabetic patients, including the Fenofibrate Intervention and Endpoint Lowering in Diabetes (FIELD) and Action to Control Cardiovascular Risk in Diabetes (ACCORD) studies.63,64 Both included participants who were predominantly White. In the FIELD study, fenofibrate did not significantly reduce the primary outcome of coronary events, but it did reduce total CVD events due to non-fatal MI and revascularizations, but benefits were seen in specific subgroups i.e., with triglycerides >204 mg/dL and HDL-C <34 mg/dL.63 In the ACCORD study, fenofibrate and simvastatin did not reduce the rate of fatal CVD events, non-fatal MI, or non-fatal stroke compared with simvastatin alone.64 Post hoc analysis of the ACCORD study reported exactly similar findings to subgroup analysis of the FIELD study. 65
PCSK-9 InhibitorsProprotein convertase subtilisin/kexin type 9 (PCSK-9) is a protease that promote the degradation of LDL receptors. PCSK-9 inhibitors are a newer class of drugs that effectively lower LDL-C levels. The Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Patients With Elevated Risk (FOURIER) trial used evolocumab, a monoclonal antibody that inhibited PCSK-9 and evaluated its effects on clinical outcomes in patients with CVD in a predominantly white population.66Compared with placebo, the mean percent reduction in LDL-C levels in patients taking evolocumab was 59%. Evolocumab treatment reduced the risk of CVD death, MI, stroke, hospitalization for unstable angina, or revascularization (9.8% vs. 11.3%; hazard ratio, 0.85; 95% CI, 0.79 to 0.92; p<0.001) and the key secondary end point which included CVD death, MI, or stroke (5.9%vs. 7.4%; hazard ratio, 0.80; 95% CI, 0.73 to 0.88; p<0.001). 62 The ODYSSEY OUTCOMES (Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab) trial where alirocumab, taken every other week, reduced ischemic events significantly, including myocardial infarction and all-cause mortality when compared with placebo among patients with an acute coronary syndrome in the preceding 1–12 months.67 The primary outcome (CAD death, MI, ischemic stroke, unstable angina) for alirocumab compared with placebo was 9.5% vs. 11.1%, hazard ratio (HR) 0.85, 95% CI 0.78–0.93, p<0.001. Both these large studies included participants that were predominantly White. Further studies in SAs are needed to evaluate if similar reductions in LDL-C and overall mortality benefit are seen with use of PCSK-9 inhibitors. SAs are a high-risk group so for those patients with LDL-C >70 mg/dL despite being on maximal tolerated statin plus ezetimibe, PCSK-9 inhibitors should be considered to help LDL-C reduction to achieve goal levels.
Conclusion
The abnormal lipid profile in SAs include more atherogenic LDL-C even without significant elevations in LDL-C levels, low and dysfunctional HDL, elevated triglycerides related to insulin resistance, and high Lp(a) levels compared with whites. For any given LDL-C, SAs exhibit a higher risk for CAD. For management of dyslipidaemia, the Western guidelines including AHA/ACC/Multi-Society 2018 lipid guidelines that included SAs as a risk-enhancing factor serve as an updated guide to manage SAs with abnormal lipid profiles and elevated ASCVD risk.
Declaration of conflicting interests
The author declares no conflict of interest.
Funding
No funds were received for the study and publishing of this article.
References
1. American Community Survey. B02015 ACS Asian Alone by Selected Groups, 2017 ACS 1-Year Estimates. 2017; 2018.
2. Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996; 48(4):343-53.
3. Talegawkar SA, Jin Y, Kandula NR, Kanaya AM. Cardiovascular health metrics among south Asian adults in the United States: prevalence and associations with subclinical atherosclerosis. Prev Med. 2017; 96:79-84.
4. Kanaya AM, Vittinghoff E, Lin F, Kandula NR, Herrington D, Liu K, et al. Incidence and progression of coronary artery calci-um in south Asians compared with 4 race/ethnic groups. J Am Heart Assoc. 2019; 8(2):e011053.
5. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364(9438):937-52.
6. Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians com-pared with individuals in other countries. JAMA. 2007; 297(3):286-94.
7. Enas EA, Mehta J. Malignant coronary artery disease in young Asian Indians: thoughts on pathogenesis, prevention, and ther-apy. Coronary Artery Disease in Asian Indians (CADI) Study. Clin Cardiol. 1995; 18(3):131-135.
8. Enas EA. Coronary artery disease epidemic in Indians: a cause for alarm and call for action. J Indian Med Assoc. 2000; 98(11):694-5, 697-702.
9. Ahmed ST, Rehman H, Akeroyd JM, Alam M, Shah T, Kalra A, et al. Premature coronary heart disease in South Asians: burden and determinants. Curr Atheroscler Rep. 2018; 20(1):6.
10. Bhupathiraju SN, Guasch-Ferré M, Gadgil MD, Newgard CB, Bain JR, Muehlbauer MJ, et al. Dietary patterns among Asian Indians living in the United States have distinct metabolomic profiles that are associated with cardiometabolic risk. J Nutr. 2018; 148(7):1150-159.
11. Talegawkar SA, Kandula NR, Gadgil MD, Desai D, Kanaya AM. Dietary intakes among South Asian adults differ by length of residence in the USA. Public Health Nutr. 2016; 19(2):348-55.
12. Gadgil MD, Anderson CAM, Kandula NR, Kanaya AM. Dietary patterns are associated with metabolic risk factors in South Asians living in the United States. J Nutr. 2015;145(6):1211-217.
13. Shah AD, Vittinghoff E, Kandula NR, Srivastava S, Kanaya AM. Correlates of prediabetes and type II diabetes in US South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Ann Epidemiol. 2015; 25(2):77-83.
14. Kandula NR, Kanaya AM, Liu K, Lee JY, Herrington D, Hulley SB, et al. Association of 10-year and lifetime predicted cardio-vascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc. 2014; 3(5):e001117.
15. Karthikeyan G, Teo KK, Islam S, McQueen MJ, Pais P, Wang X, et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: an analysis from the INTERHEART Study. J Am Coll Cardiol. 2009; 53(3):244-53.
16. Kalhan R, Puthawala K, Agarwal S, Amini SB, Kalhan SC. Altered lipid profile, leptin, insulin, and anthropometry in offspring of South Asian immigrants in the United States. Metabolism. 2001; 50(10):1197-202.
17. Anand SS, Yusuf S, Vuksan V, Devanesen S, Montague P, Kelemen L, et al. The Study of Health Assessment and Risk in Ethnic groups (SHARE): rationale and design. The SHARE Investigators. Can J Cardiol. 1998; 14(11):1349-357.
18. Hastings KG, Jose PO, Kapphahn KI, Frank ATH, Goldstein BA, Thompson CA, et al. Leading causes of death among Asian American subgroups (2003-2011). PLoS One. 2015; 10(4): e0124341.
19. Barzi F, Patel A, Woodward M, Lawes CM, Ohkubo T, Gu D, et al. A comparison of lipid variables as predictors of cardiovas-cular disease in the Asia Pacific region. Ann Epidemiol. 2005; 15(5):405-13.
20. Thomas I, Gupta S, Sempos C, Cooper R. Serum lipids of Indian physicians living in the U.S. compared to U.S.-born physi-cians. Atherosclerosis. 1986; 61(2):99-106.
21. Krishnaswami S, Prasad NK, Jose VJ. A study of lipid levels in Indian patients with coronary arterial disease. Int J Cardiol. 1989; 24(3):337-45.
22. St-Pierre AC, Cantin B, Dagenais GR, Mauriège P, Bernard PM, Després JP, et al. Low-density lipoprotein subfractions and the long-term risk of ischemic heart disease in men: 13-year followup data from the Quebec Cardiovascular Study. Arterioscler Thromb Vasc Biol. 2005;25(3):553-59.
23. Kulkarni KR, Markovitz JH, Nanda NC, Segrest JP. Increased prevalence of smaller and denser LDL particles in Asian Indians. Arterioscler Thromb Vasc Biol. 1999; 19(11):2749-755.
24. Palaniappan LP, Kwan AC, Abbasi F, Lamendola C, McLaughlin TL, Reaven GM. Lipoprotein abnormalities are associated with insulin resistance in South Asian Indian women. Metabolism. 2007; 56(7):899-904.
25. Dodani S. Excess coronary artery disease risk in South Asian immigrants: can dysfunctional high-density lipoprotein explain increased risk? Vasc Health Risk Manag. 2008; 4(5):953-61.
26. Ehtisham S, Crabtree N, Clark P, Shaw N, Barrett T. Ethnic differences in insulin resistance and body composition in United Kingdom adolescents. J Clin Endocrinol Metab. 2005; 90(7):3963-969.
27. Bakker LEH, Boon MR, Annema W, Dikkers A, van Eyk HJ, Verhoeven A, et al. HDL functionality in South Asians as com-pared to white Caucasians. Nutr Metab Cardiovasc Dis. 2016; 26(8):697-705.
28. Chow CK, McQuillan B, Raju PK, Iyengar S, Raju R, Harmer JA, et al. Greater adverse effects of cholesterol and diabetes on carotid intima-media thickness in South Asian Indians: comparison of risk factor-IMT associations in two population-based surveys. Atherosclerosis. 2008; 199(1):116-22.
29. Dodani S, Dong L, Guirgis FW, Reddy ST. Carotid intima media thickness and low high-density lipoprotein (HDL) in South Asian immigrants: could dysfunctional HDL be the missing link? Arch Med Sci. 2014; 10(5):870-79.
30. Bhalodkar NC, Blum S, Rana T, Bhalodkar A, Kitchappa R, Kim KS, et al. Comparison of levels of large and small high-density lipoprotein cholesterol in Asian Indian men compared with Caucasian men in the Framingham Offspring Study. Am J Cardiol. 2004; 94(12):1561-563.
31. Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in south Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabeto-logia. 2006; 49(11):2580-588.
32. Dodani S, Henkhaus R, Wick J, Vacek J, Gupta K, Dong L, et al. Metabolic syndrome in South Asian immigrants: more than low HDL requiring aggressive management. Lipids Health Dis. 2011; 10:45-5.
33. Superko HR, Enas EA, Kotha P, Bhat NK, Garrett B. High-density lipoprotein subclass distribution in individuals of Asian Indian descent: The National Asian Indian Heart Disease Project. Prev Cardiol. 2005; 8(2):81-6.
34. Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes. 2011; 35(2):167-87.
35. Ajjan R, Carter AM, Somani R, Kain K, Grant PL. Ethnic differences in cardiovascular risk factors in healthy Caucasian and South Asian individuals with the metabolic syndrome. J Thromb Haemost. 2007; 5(4):754-60.
36. Petersen KF, Dufour S, Feng J, Befroy D, Dziura J, Man CD, et al. Increased prevalence of insulin resistance and nonalcoholic fatty liver disease in Asian-Indian men. Proc Natl Acad Sci U S A. 2006; 103(48):18273-8277.
37. Shah AD, Kandula NR, Lin F, Allison MA, Carr J, Herrington D, et al. Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes. 2016; 40(4):639-45.
38. Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan NP. Racial/ethnic differences in dyslipidemia patterns. Circu-lation. 2014; 129(5):570-79.
39. Sandhofer A, Kaser S, Ritsch A, Laimer M, Engl J, Paulweber B, et al. Cholesteryl ester transfer protein in metabolic syndrome. Obesity (Silver Spring). 2006; 14(5):812-18.
40. Rashid S, Sniderman A, Melone M, Brown PE,Otvos JD, Mente A, et al. Elevated cholesteryl ester transfer protein (CETP) activity, a major determinant of the atherogenic dyslipidemia, and atherosclerotic cardiovascular disease in South Asians. Eur J Prev Cardiol. 2015; 22(4):468-77.
41. Clarke R, Peden JF, Hopewell JC, Kyriakou T, Goel A, Heath SC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009; 361(26):2518-528.
42. Erqou S, Kaptoge S, Perry PL, Di Angelanonio E, Thompson A, White IR, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009; 302(4):412-23.
43. Kamstrup PR, Typjaerg-Hansen A, Steffenson R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009; 301(22):2331-339.
44. Gambhir JK, Kaur H, Gambhir DS, Prabhu KM. Lipoprotein(a) as an independent risk factor for coronary artery disease in patients below 40 years of age. Indian Heart J. 2000; 52(4):411-15.
45. Anand SS, Enas EA, Pogue J, Haffner S, Pearson T, Yusuf S. Elevated lipoprotein(a) levels in South Asians in North America. Metabolism. 1998; 47(2):182-84.
46. Banerjee D, Wong EC, Shin J, Fortmann SP, Palaniappan L. Racial and ethnic variation in lipoprotein (a) levels among Asian Indian and Chinese patients. J Lipids. 2011; 2011:291954.
47. Palaniappan L, Anthony MN, Mahesh C, Elliott M, Killeen A, Giacherio D, et al. Cardiovascular risk factors in ethnic minority women aged < or =30 years. Am J Cardiol. 2002; 89(5):524-29.
48. Velmurugan K, Deepa R, Ravikumar R, Lawrence JB, Anshoo H, Senthilvelmurugan M, et al. Relationship of lipoprotein(a) with intimal medial thickness of the carotid artery in type 2 diabetic patients in south India. Diabet Med. 2003; 20(6):455-61.
49. Giri S, Dwivedi S. Lipoprotein (a) and lipid levels in young patients with myocardial infarction and their first-degree relatives. Indian Heart J. 2002; 54(1):110.
50. Pare G, Caku A, McQueen M, Anand SS, Enas E, Clarke R, et al. Lipoprotein(a) levels and the risk of myocardial infarction among seven ethnic groups. Circulation. 2019; 139:1472-482.
51. Kanaya AM, Kandula N, Herrington D, Budoff MJ, Hulley S, Vittinghoff E, et al. Mediators of Atherosclerosis in South Asians Living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol. 2013; 36(12):713-20.
52. Olson JL, Bild DE, Kronmal RA, Burke GL. Legacy of MESA. Glob Heart. 2016; 11(3):269-74.
53. Huffman MD, Kandula NR, Baldridge AS, Tsai MI, Prabhakaran D, Kanaya AM. Evaluating the potential association between lipoprotein(a) and atherosclerosis (from the mediators of atherosclerosis among South Asians living in America cohort). Am J Cardiol. 2019; 123(6):919-921.
54. Wilson PWF, Polonsky TS, Miedema MD, Khera A, Kosinski AS, Kuvin JT. Systematic review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a re-port of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019; 73(24):3210-3227.
55. Chandra KS, Bansal M, Nair T, Iyenger SS, Gupta R, Manchanda SC, et al. Consensus statement on management of dyslipid-emia in Indian subjects. Indian Heart J. 2014; 66(Suppl 3):S1-51.
56. Gupta M, Braga MFB, Teoh H, Tsigoulis M, Verma S. Statin effects on LDL and HDL cholesterol in South Asian and white populations. J Clin Pharmacol. 2009; 49(7):831-37.
57. Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, et al. Cholesterol lowering in intermediate-risk persons without cardio-vascular disease. N Engl J Med. 2016; 374(21):2021-031.
58. Lee E, Ryan S, Birmingham B, Zalikowski J, March R, Ambrose H, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin Pharmacol Ther. 2005;78(4):330-41.
59. Mahadevan L, Yesudas A, Sajesh PK, Revu S, Kumar P, Santhosh D, et al. Prevalence of genetic variants associated with car-diovascular disease risk and drug response in the Southern Indian population of Kerala. Indian J Hum Genet. 2014; 20(2):175-84.
60. Menon AS, Singh Y,Kotwal N, Girish R. Statins: cholesterol guidelines and Indian perspective. Indian J Endocr Metab. 2015; 19(5):546-53.
61. Jia L, Betters JL, Yu L. Niemann-pick C1-like 1 (NPC1L1) protein in intestinal and hepatic cholesterol transport. Annu Rev Physiol. 2011; 73:239-59.
62. Madan M, Vira T, Rampakakis E, Gupta A, Khithani A, Balleza L, et al. A randomized trial assessing the effectiveness of ezetimibe in South Asian Canadians with coronary artery disease or diabetes: the INFINITY study. Adv Prev Med. 2012; 2012:103728.
63. Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovas-cular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005; 366(9500):1849-861.
64. Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362(17):1563-1574.
65. Elam M, Lovato L, Ginsberg H. The ACCORD-Lipid study: implications for treatment of dyslipidemia in type 2 diabetes mel-litus. Clinical lipidol. 2011; 6(1):9-20.
66. Sabatine MS, Giugliano RP, Keech AC, Honarpour N,Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017; 376(18):1713-1722.
67. Maki KC. The ODYSSEY Outcomes trial: clinical implications and exploration of the limits of what can be achieved through lipid lowering. J Clin Lipidol. 2018; 12(5):1102-105.
