
Case Series
 Clinical Profile and Laboratory Parameters in Diabetic and Non-Diabetic COVID-19 Patients
Clinical Profile and Laboratory Parameters in Diabetic and Non-Diabetic COVID-19 Patients
Abstract
Objective: COVID-19 infection has spread across the world and caused numerous casualties more so in elderly people with pre-existing chronic diseases. Diabetes mellitus with COVID-19 infection shows multifold increase in mortality.
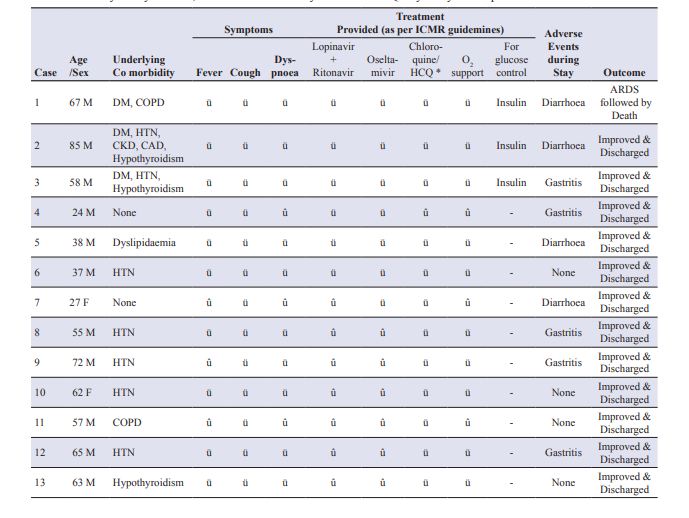
Brief Report Presentation: We share a data of 13 cases with COVID-19 pneumonia out of which 3 patients were diabetic and 10 patients without diabetes. Our aim is to compare and share their clinical findings, biological parameters and inflammatory markers along with the treatment administered stressing on the imperative need to control blood sugar levels as well.
Conclusion: COVID-19 patients with diabetes constitute a high risk group and have a greater baseline elevation in pro inflammatory markers than patients without diabetes. These biomarkers may be used for assessing disease severityin COVID-19 patients and also help in disease stratification of patients in which aggressive therapeutic approach is required.
Keywords
Introduction
The catastrophic consequences of unabated spread of COVID-19 continue to wreak havoc across the globe. Majority of the deaths have occurred in people who were aged 65 and above and patients with underlying co morbidities such as diabetes mellitus, hypertension, cardiovascular diseases, chronic kidney disease and respiratory diseases.1 It is imperative to understand why diabetic patients are more vulnerable of contracting the disease, have serious complications and ultimately have a high risk of mortality as compared to the general population. This is essential because India is the home to every 6th diabetic individual in the world, comprising more than 77 million diabetics and failure to contain the virus can lead to disastrous consequences and death toll may reach mammoth proportions.2 Many previous studies have reported that mortality was about threefold higher in people with diabetes as compared to the general population with COVID-19 infection in China.3 In a study conducted by Guan et al. comprising of 1590 COVID-19 patients, it was found that (25.1%) reported having at least one comorbidity.1 The most prevalent comorbidity was hypertension (16.9%), followed by diabetes (8.2%). After adjusting forage and smoking status, chronic obstructive pulmonary disease (COPD) [hazards ratio (HR) 2.681, 95% confidence interval(95% CI) 1.424-5.048], diabetes (HR 1.59, 95% CI 1.03-2.45), hypertension (HR 1.58, 95% CI 1.07-2.32) and malignancy(HR 3.50, 95% CI 1.60-7.64) were risk factors of reaching to the composite endpoints.As the world continues to battle the cataclysmic effects of this pandemic, we would like to share our experiences regarding the clinical profile, laboratory evaluation and treatment of 3 diabetic patients and 10 non-diabetic patients who had COVID-19pneumonia and was admitted in Sawai Mansingh hospital (S.M.S), Jaipur, Rajasthan, India. The potential role of various inflammatory markers and dynamic changes in IL-6 (especially in diabetic patients) was tracked to assess the severity of the disease
Case Summary of Diabetic Patients with COVID-19 Pneumonia
Case 1:
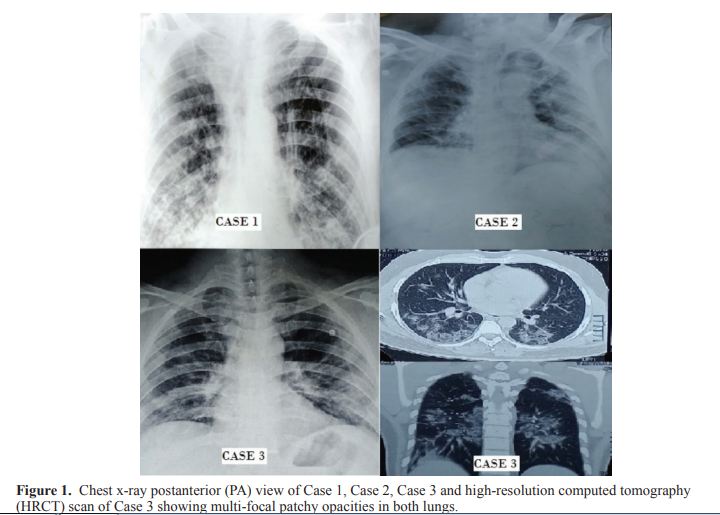
A 67-year-old diabetic male, chronic smoker (40 pack years) was admitted in S.M.S. hospital with the chief complaints of cough and sore throat since 8 days followed by fever and shortness of breath since 3 days. His throat swab tested positive for COVID-19 after 3 days. At presentation his vitals BP was 134/78 mm of Hg, pulse rate was 125/min and respiratory rate was 28/min. Respiratory system examination revealed bilateral crepitations. Other systems were normal on examination. His electrocardiogram (ECG) was suggestive of sinus tachycardia with p-pulmonale, right bundle branch block (RBBB) pattern and T wave inversions. Chest x-ray posteroanterior (PA) view (Figure 1 ) was suggestive of chronic obstructive disease (COPD) with right lower lobe pneumonitis. Haemogram showed leucocytosis with neutrophilia and lymphopenia. Markers of inflammation such as lactate dehydrogenase (LDH), C-reactive protein (CRP), pro-calcitonin (PCT), serum ferritin, fibrin degradation product (FDP) and D-dimer were elevated. Dynamic changes of interleukin-6 (IL-6) levels were observed at admission and during treatment course. Patient’s COVID-19 sample came negative on Day 12 and Day 13 of admission. Unfortunately, secondary bacterial infection in lungs landed him into acute respiratory distress syndrome (ARDS) and he needed invasive ventilator support.
Case 2:
An 85-year-old man who was a known case of diabetes mellitus (10 years), hypertension (10 years), hypothyroidism (8years), chronic kidney disease (4 years) and coronary artery disease (4 years) had history of travel to Dubai. He presented with the chief complaints of mild fever, cough, sore throat and shortness of breath and his vitals were- BP 148/82 mm of Hg, O2 saturation 84% on room air and pulse rate of 120/min. His respiratory rate was 25/min. Respiratory system examination revealed bilateral equal air entry with basal creptitations. All other system examination was normal. ECG was suggestive for RBBB pattern and poor R wave progression. Chest x-ray was suggestive of bilateral pneumonitis (Figure 1). During the period of hospitalization leucocytosis with neutrophilia and lymphopenia were seen. His renal function worsened due to concomitant infection and markers of inflammation were elevated along with IL-6 (Table 2). Throat swabs were sent regularly for COVID-19 testing which came negative on Day 5 and on Day 6 of admission. He was discharged and advised home isolation of 14 days with strict glycaemic control.
Case 3:
A 58-year-old male, health-care professional, resident of Bhilwara (Manchester of India: one of the cluster hotspots in Rajasthan) with comorbidities of hypertension, diabetes mellitus and hypothyroidism for 8 years presented with chief complaints of fever and dry cough in the past 7 days followed by shortness of breath in the past 3 days. His blood pressure(BP) was 150/90 mm of Hg and pulse rate was 97/min, O2 saturation was 90% on room air at the time of presentation. ECG was suggestive of hypertensive changes. Computed tomography (CT) scan (Figure 1 ) showed multifocal patchy peripheral and ground glass opacities in both lung parenchyma, involving both lobes suggestive of viral pneumonitis. Gradually with treatment disease remission started and symptoms ameliorated. On the 6th day of his admission, his oropharyngeal sample came negative for COVID-19 with a repeat negative after 24 hrs. He was discharged and advised home isolation for 14 days.
Case Summary of Cases 4-13 COVID-19 Pneumonia Patients Without Diabetes
Out of 10 patients without diabetes 8 were males and 2 females. The mean age of these patients was 50 years. Hypertension was present in 50% of these patients. All patients presented with cough and had consolidation in their chest X-ray suggestive of pneumonia. Out of these 7 patients presented with fever and dyspnoea. These patients needed oxygen support. Lymphopenia was observed in 70% of these patients. It was evident that baseline levels of markers of inflammation were elevated in these patients, but not to the extent seen in diabetic patients. IL-6 quantitative values showed dynamic change with patient’s disease remission. All patients improved completely after therapy and were discharged and advised home quarantine.
Treatment
Treatment of all was done as per the Indian Council of Medical Research (ICMR) guidelines with few individual changes.4 Tab. lopinavir 200 mg + ritonavir 50 mg 2 BD, Cap. oseltamivir 150 mg BD (modified according to renal clearance), tab. chloroquine 500 mg BD/tab. hydroxychloroquine 400 mg BD on Day 1 followed by 200 mg BD for 4 days along with empirical antibiotics for pneumonia (Table 1) were administered. Later, appropriate antibiotics were started according to the culture sensitivity report. All patients with diabetes were given injectable insulin for glycaemic control. Case 1 required Bilevel Positive Airway Pressure (BiPaP) support and was intubated on Day 12 when his condition deteriorated and he landed into ARDS. Case 2 and Case 3 were able to maintain oxygen saturation with the help of low flow oxygen mask delivering oxygen at the rate of 1 L/min. Case 5 and 6 needed high flow oxygen mask for maintaining oxygen saturation. Other non-diabetic patients were able to maintain saturation on normal oxygen mask. Cases 4, 7 and 11 did not require oxygen support.Target oxygen saturation was kept at 95%.
Discussion
It was observed that in diabetic patients with COVID-19 pneumonia, there was a comparatively greater elevation in baseline levels of markers of inflammation as compared to COVID-19 pneumonia patients without diabetes (Table 2).
The severity of COVID-19 is increased in diabetes, perhaps because this disease is itself a pro-inflammatory state and causes impairment in the body’s response to all kinds of infections. Alterations have been noted in macrophage activation and release and action of various cytokines. Patients with uncontrolled diabetes not only show poor response to viral infections but alsoto any secondary infection caused by bacteria. When cells were observed, it was seen that microorganisms adhere more and densely in diabetes as compared to non-diabetics.5,6 Poorly controlled diabetes shows renal and cardiac complications which can be implicated in the worsening of COVID-19 symptoms. Studies show decreased functions (chemotaxis and phagocytosis)of diabetic polymorphonuclear cells and diabetic monocytes/macrophages.7 Moreover, some microorganisms become more virulent in a high glucose environment.
Due to an unhealthy lifestyle, obesity is increasing worldwide. It is alarming because it is a risk factor for both diabetes and infection.8 Reports from the 2009 epidemic of H1N1 suggest that the severity of infection was two times higher among the obese population.9 Abdominal obesity also shows changes in the secretory pattern of cytokines and adipocytes thus harming the immune activity of the body.10 Obese people have breathing difficulties and poor gas exchange in the basal part.The accumulated secretions also increase the risk of infections.11

Some concerns have arisen regarding the use of angiotensin-converting enzymes (ACE) inhibitors in hypertensive diabetics. Coronavirus binds to target cells through ACE2 receptors.12 In patients treated with ACE and angiotensin II receptor blockers, expression of ACE2 is upregulated, thus increasing ACE2 expression and this facilitates increased infection withCOVID-19.13 Thus, the use of ACE2-stimulating drugs would facilitate the entry of SARS-CoV-2 into pneumocytes and might result in more severe and fatal diseases.14 Strangely reduced ACE2 expression might also predispose to severe lung injury and ARDS with COVID-19 as seen in patients with diabetes mellitus possibly due to glycosylation of ACE2.15 However, the American Heart Association (AHA), the European Society of Cardiology (ESC) and the International Society of Hypertension (ISH) recommend to continue use of ACE inhibitors and angiotensin receptor blockers (ARBs) in managing hypertension inpatients with COVID-19 infection, due to scarcity of concrete adverse data.16-18
With more and more countries enforcing lockdown to combat COVID-19 spread, the anxiety levels have shot up due tothe spread of the global pandemic. Stress causes a decrease in insulin level and increases its antagonistic hormones which cancontribute to stress-induced hyperglycaemia.19
The key to the management of diabetic patients with COVID-19 infection is to maintain adequate glycaemic control as hyperglycaemia is a major factor determining morbidity and mortality in these patients. Even though injectable insulin remains the mainstay of treatment in patients with severe disease, but patients who are asymptomatic or having mild symptoms can continue their oral anti-diabetic drug. Though metformin should be used cautiously during an acute infection and it may be necessary to temporarily stop it in severe infection and dehydration. Recent preclinical and clinical studieshave suggested that metformin not only improves chronic inflammation through the improvement of metabolic parameters such as hyperglycaemia, insulin resistance and atherogenic dyslipidaemia, but also has a direct anti-inflammatory action by inhibition of nuclear factor κB (NFκB) via AMP-activated protein kinase (AMPK)-dependent and independent pathways.20Dipeptidyl peptidase-4 (DPP-4) has been identified as a co-receptor for Middle East Respiratory Syndrome coronavirus (MERS). DPP-4 activity also potentially modulates the levels and function of multiple immunomodulatory chemokines and cytokines. However, the effects of DPP-4 inhibition on the immune response in patients with type 2 diabetes is controversial and not completely understood.21 Sodium-glucose co-transporter-2 (SGLT-2) inhibitors need to be used with precaution due to the adverse effect of dehydration and euglycemic ketoacidosis. Sulphonylureas may induce hypoglycaemia in patients with low-calorie intake. Besides anti-diabetic drugs, patients should be advised about a balanced diet and exercising regularly. This will help in maintaining optimum glycaemic control and also alleviate anxiety
Elderly patients especially those with diabetes show severe lung injury due to initiation of a cascade of inflammatory reactions resulting in the cytokine storm syndrome. This leads to unbridled inflammation resulting in uncontrolled liberation of cytokines like IL -6 and dysregulation of feedback mechanisms.22,23 Other inflammatory markers such as procalcitonin, serum ferritin, CRP, LDH, FDP, D-dimer were also found elevated in our study and studies done previously.24 In our study,we found that baseline IL-6 levels were elevated in COVID-19 patients and they were comparatively greater in patients with diabetes as compared to non-diabetic patients. Moreover, IL-6 displayed dynamic changes in its quantitative levels with remission or aggravation of the disease suggesting that this marker may play a role in the prognosis of the disease.
The mean duration of getting 1st and 2nd COVID-19 report negative was 8.3 days and 9.5 days respectively in patients without diabetes while it was 7.6 days and 8.6 days, respectively in patients with diabetes. Possible explanation of shorter period in diabetics was probably due to lesser mean age in the non-diabetes group. All patients in the non-diabetes group recovered completely and were discharged with an undertaking for home/ centre quarantine, whereas 1 patient who had diabetes developed ARDS and succumbed to the illness.
Conclusion
PAs the global pandemic of COVID-19 continues to rage on it is imperative that patients of diabetes mellitus adopt a healthy lifestyle with strict adherence to diabetic diet, monitor blood sugar levels regularly and accordingly follow the treatment advised by the doctor. Ensuring strict glycaemic control is of paramount importance in ensuring better outcomes in diabetic patients with COVID-19 infection with injectable insulin remaining the mainstay of treatment. Patients who are asymptomatic or having only mild disease may require some modifications in their anti-diabetic drugs dose/type. Practising Yoga and exercising regularly at home can also help in maintain glycaemic control. Markers of inflammation were elevated to a greater level inpatients with diabetes when compared to patients without diabetes and IL-6 displayed dynamic changes with disease progression and remission and may have a role as a prognositic marker though more studies are needed for conclusive evidence.
Acknowledgements
We acknowledge guidance of Dr. Subarta Banerjee, Dr. Raman Sharma and Dr. Ajit Singh Shaktawat, members of treatment panel of COVID-19 of S.M.S. Hospital, Jaipur, India. We also acknowledge Dr. Arpit Gupta, Dr. Ankita Kharadi and Dr. Kamlesh Parihar for their contribution in data collection and Mr. Arif Khan for computer related tasks.
Declaration of Conflicting Interest
The authors do not have any conflict of interest.
Ethical Approval
Ethics approval issue was discussed with committee, as per them wording approval is not required for case series/case report.
Informed Consent
Written informed consent for health record sharing was taken by all patients.
Funding
No funds were received for the study and publishing.
References
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A Nationwide Analysis. Eur Respir J. 2020.
- Ramchandran A, Snehlata C , Kapur A. Vijay V, Mohan V, Das A K, et al. High prevalence of diabetes and impaired glucose tolerance in India: National urban Diabetes Survey. Diabetologia. 2001; 44(9):1094-101.
- Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. The clinical course and outcome of critically ill patients with SARS-CoV-2 in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020; pii: S2213-2600(20)30079-5.
- Bhatnagar T, Murhekar MV, Soneja M, Gupta N, Giri S, Wig N, et al. Lopinavir/ritonavir combination therapy amongst symptomatic coronavirus disease 2019 patients in India: Protocol for restricted public health emergency use. Indian J Med Res. 2020.
- Ferlita S, Yegiazaryan A, Noori N, Lal G, Nguyen T, To K, et al. Type 2 diabetes mellitus and altered immune system leading to susceptibility to pathogens, especially with mycobacterium tuberculosis. J Clin Med. 2019; 8(12). pii: E2219.
- Aly FZ, Blackwell CC, Mackenzie DAC, Weir DM, Clarke F. Factors influencing oral carriage of yeasts among individuals with diabetes mellitus. Epidemiol Infect. 1992; 109(3):507-18.
- Geerlings SE, Hopelman AIM. Immune dysfunction in patients with diabetes mellitus, FEMS Immunology and Medical Microbiology. 1999; 26(03-4): 259-65.
- Huttunen R, Syrjanen J. Obesity and the risk and outcome of infection. Int J Obes (Lond). 2013; 37(3):333-40.
- Wu Z, McGoogan JM. Characterstics and important lessons from the corona virus disease 2019 outbreak in China: summary of a report of 72314 cases from the Chinese Centre for Disease Control and Prevention. JAMA. 2020.
- Kang YE, Kim JM, Joung KH, Lee JH, You BR, Choi MJ, et al. The roles of adipokines, proinflammatory cytokine, and adipose tissue macrophages in obesity associated insulin resistance in modest obesity and early metabolic dysfunction. PLoS One. 2016; 11(4):e0154003
- Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018; 12(9):755-767.
- Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE-2 and TMPRSS-2 and is blocked by a clinically proven protease inhibitor. Cell. 2020; 181(2):271-280.e8.
- Li XC, Zhang J, Zhuo JL. The vasoprotective axes of the renin-angiotensin system (RAAS): Physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases. Pharmacol Res. 2017; 125(Pt A):21-38.
- Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection. Lancet Respir Med. 2020; 8(4):e21.
- Pal R, Bhansali A. COVID-19, diabetes mellitus and ACE2: The conundrum. Diabetes Res Clin Pract. 2020 Apr; 162: 108132
- American College of Cardiology. HFSA/ACC/AHA statement addresses concerns regarding reusing RAAS antagonists in COVID-19. Available at https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-COVID-19.
- European Society of Cardiology. Position statement of the ESC Council on Hypertension on ACE-Inhibitors(ACE-I) and Angiotensin Receptor Blockers (ARBs). Available at https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang.
- International Society of Hypertension. A Statement given by the International Society of Hypertension on COVID-19. Available at https://ish-world.com/news/a/A-statement-from-the-International-Society-of-Hypertension-on-COVID-19/.
- Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011; 15(1):18-22.
- Yoshifumi S. Metformin and Inflammation: Its potential beyond Glucose lowering effect. Endocr Metab Immune Disord Drug Targets. 2015; 15(3):196-205.
- Iacobellis G. COVID-19 and diabetes: Can DPP-4 inhibtion play a role? Diabetes Res Clin Pract. 2020; 162:108125.
- Paquette SG, Banner D, Zhao Z, Fang Y, Huang SS, Leόn AJ, et al. Interleukin-6 is a Potential Biomarker for Severe Pandemic H1N1 Influenza A Infection. PLoS One. 2012; 7(6): e38214.
- Wang Y, Wang Y, Chen Y, Qin Q, et al. Unique epidemiological and clinical feature of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020.
- Mehta P, McAuley D, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395(10229):1033-1034.
