
Review
Abstract
Lipid abnormalities, including high levels of low-density lipoprotein (LDL) cholesterol, elevated triglycerides (TGs) and low levels of high-density lipoprotein (HDL) cholesterol, are associated with an increased risk of primary as well secondary cardio vascular (CV) events. Reduction of elevated LDL certainly gives mortality benefit, but some residual CV risk factors like abnormal life style, uncontrolled co-morbid conditions like hypertension, diabetes mellitus and elevated TG level may increase CV mortality in spite of low LDL. TG >200 mg/dL needs to be controlled by statin and other TG lowering drugs. High TG contributes not only for CV mortality but also leads to non-alcoholic fatty liver disease (NAFLD) which is commonly seen in obese and diabetic patients. Recently, the European guidelines are also in favour to reduce elevated TG when it is between 135-499 mg/dL in high risk patients. In India, elevated TG is more common pattern of dyslipidaemia, compared to western world and still its optimized reduction through TG lowering drugs is not done at regular basis. Saroglitazar is first dual PPAR agonist drug which has shown significant TG reduction diabetic dyslipidaemia patients with better glycaemic control and safety profile.
Keywords
Keywords: Saroglitazar, hypertriglyceridemia, diabetic dyslipidaemia, PPAR, residual CV risk
Introduction
Lipid abnormalities, including high levels of low-density lipoprotein (LDL) cholesterol, elevated triglycerides (TGs) and low levels of high-density lipoprotein (HDL) cholesterol are associated with an increased risk of primary as well secondary cardio vascular (CV) events.1 According to international and national guidelines, lowering LDL with a statin is a primary objective to prevent both primary and secondary CV disease prevention.2 Various meta-analysis of statin studies had shown that as statin dose is increased, LDL level and CV events both are reduced significantly. But along with that many studies had also shown that despite control on LDL level with high dose of statin, patients may have 60-70% residual CV risk factor. Beyond LDL, many factors are contributing to residual CV risk like abnormal life style, uncontrolled co-morbid conditions like hypertension, diabetes mellitus, elevated TG level, etc.3 In management of dyslipidaemia, few patients, especially South Asians may have elevated TG >200 mg/dL in spite of controlled LDL after statin, which can increase CV events. In this scenario, guidelines have difference in opinion on adding TG lowering agent along with statin to prevent CVD.4 High TG is not associated with only CVD, but along with that it may increase risk of non-alcoholic fatty liver disease (NAFLD) and acute pancreatitis as well.5 So, TG lowering may be a cornerstone therapy along with /- or without statin for treatment of CVD and other complications as mentioned above.6
Epidemiology of Hypertriglyceridaemi
Dyslipidaemia is defined as abnormal level of lipoprotein lipid such as high total cholesterol, low density lipoprotein (LDL) cholesterol, very low density lipoprotein (VLDL) cholesterol and triglycerides and low high density lipoprotein (HDL). Dyslipidaemia has strong association with CVD, especially with high LDL.7 LDL lowering through statin is a primary objective for any high risk CV patients, but even in patients with controlled LDL, may have residual CV risk due to multiple factors like abnormal life style, uncontrolled co-morbid conditions like hypertension, diabetes mellitus, elevated TG level, etc.3 High TG is a critical risk factor for CVD and other metabolic conditions, but due to lack of support from international guidelines, TG reduction therapy is frequently ignored by clinicians in spite of multiple evidences which show that high TG leads to atherosclerosis, NAFLD, acute pancreatitis, etc.5
According to the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III), elevated triglyceride is defined as 150 mg/dL and higher. According to these criteria, the Third National Health and Nutrition Examination Survey (NHANES) found that the prevalence of hypertriglyceridaemia in US adults was approximately 35% in men and 25% in women.8 Like western population, India is undergoing for rapid transition in socio-economic sector, life style improvement and aging associated disease. The Jaipur Heart Watch (JHW) review studies in India showed secular trend in increasing lipid abnormality over duration of 12 years. It was observed insignificant increment change in cholesterol lipid like LDL and HDL, while it was significant incremental change in triglyceride level was observed (Figure 1). The study also reported a significant association of increasing dyslipidaemias with increasing truncal obesity and obesity.7,9
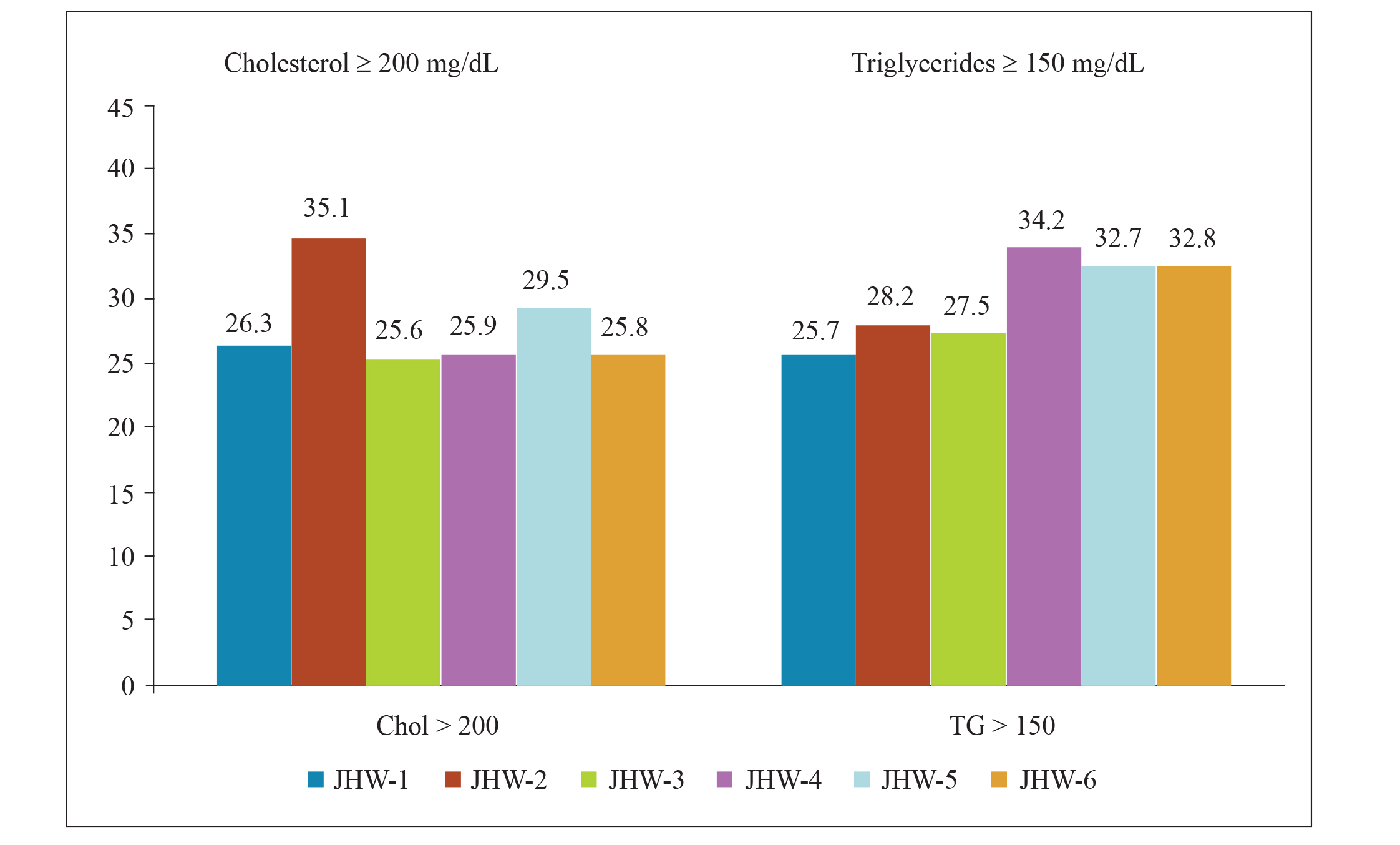
Figure 1. 20 years trend of cholesterol and triglyceride level in urban Indian population7
The Indian Council of Medical Research India Diabetes Study (ICMR INDIAB) phase I, involving three states and one union territory (UT), representing the north, south, east and west of the country had presented dyslipidaemia pattern in 2,042 Indian population which is covering 213 million Indian population from respective area.10 Results were showing that 8 out of 10 Indian adults have dyslipidaemia (Figure 2) and most common pattern of dyslipidaemia was low HDL (72.3%) followed by High TG (29.5%), high cholesterol (13.9%) and high LDL (11.8%).
This is very frequently seen in Asian Indian phenotype, which also includes increased truncal adiposity, increased insulin level, increased insulin resistance, higher hip waist circumference ratio, etc.11 So in India, with such wide population dyslipidaemia, high TG also plays vital role in development of CV disease.
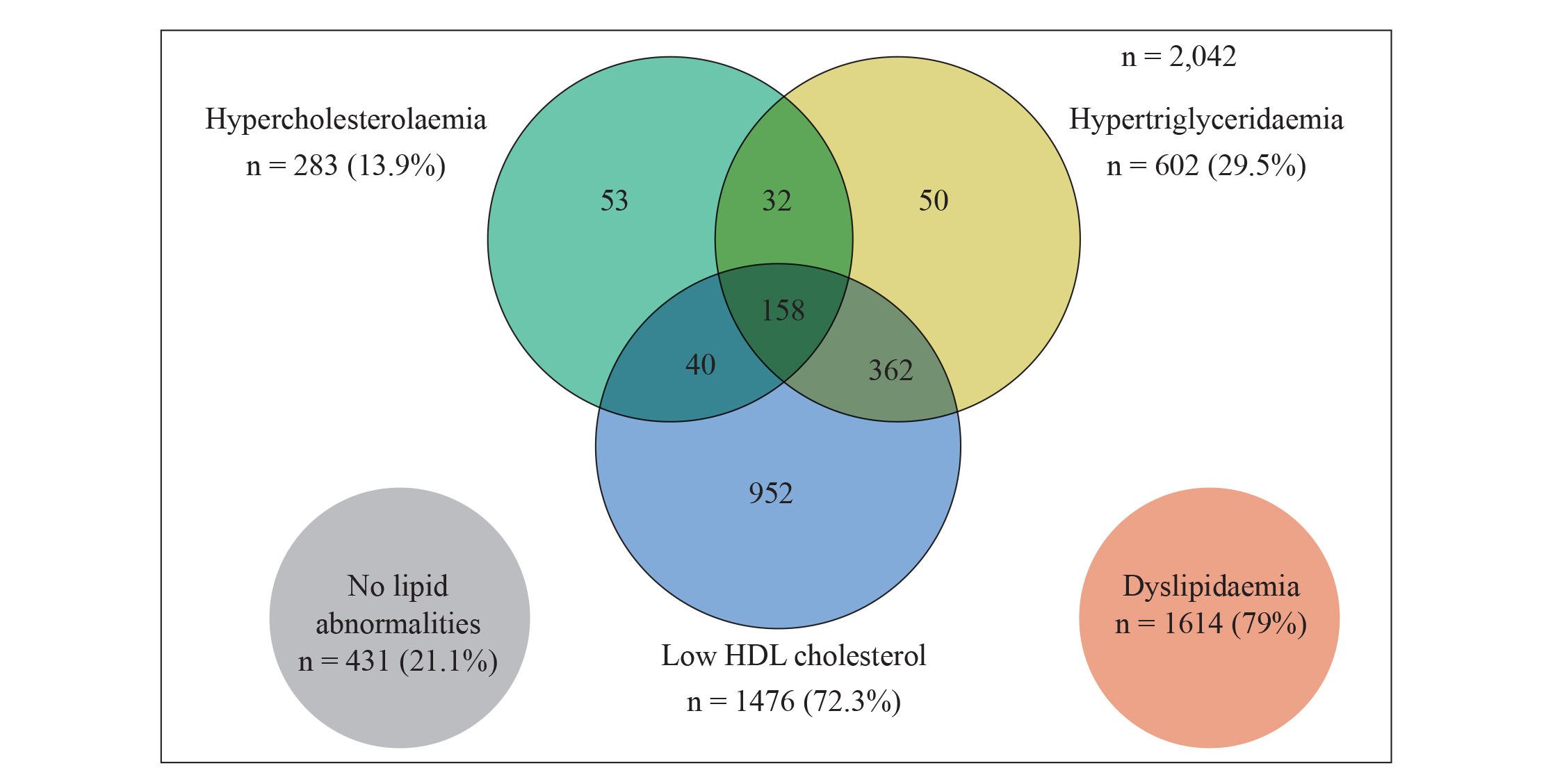
Figure 2. Overlapping pattern of dyslipidaemia in Indian population10
Residual Cardio Vascular (CV) Risk in Statin Treated Patient
Statins are always considered as the first line therapy for dyslipidaemia to decrease LDL levels and risk of cardiovascular disease (CVD) both. But in spite of statin therapy, residual CV risk factor still remains due to low HDL and high TG.12 The Scandinavian Simvastatin Survival Study (4S) of patients with known coronary heart disease and high levels of LDL, had shown significant reduction of CV events with statin treatment compared to placebo, however, a 20% CV event rate was noted in statin treated patients.13 Kearny PM et al. (2008) reported from meta-analysis of 14 trials involving 18,686 people with diabetes with statin therapy, that low HDL and high triglyceride limits the efficacy of statin therapy alone in reducing the vascular events despite achieving target LDL levels. In various statin studies, it is observed that post statin therapy with controlled LDL, residual CV risk still remains ~60-70% in patients, where in elevated TG is one of the important risk factor. Apart from this, many studies have proven that Indian have higher TG levels along with low HDL, which are major risk factors for increasing CVD risk .14-17
Elevated Triglyceride (TG >200 mg/dL) is a CV Risk Factor
Elevated TG is an independent CV risk factor, which is proven by Sarwar et al., in meta-analysis of data from 2,62,525 participants from 29 studies. 18 In their analysis, it was observed that high TG is strongly associated with CV disease which was independent of follow-up duration, age and fasting. Moreover, this data predated completion of PROVE IT-TIMI 22 trial, where in analysis revealed that high TG is considerable risk factor with irrespective of LDL level in acute coronary syndrome (ACS) patients. It was also observed, the reduced risk of coronary heart disease (CHD) with low on-treatment TG (<150 mg/ dL). For each 10 mg/dL decline in on treatment TG, there was a 1.6% lower risk of the composite end point (p <0.001) after adjustment for LDL and other covariates. Moreover, the combination of low LDL (<70 mg/dL) and low TG (<150 mg/dL) was associated with the lowest event rates compared with higher LDL, higher TG or both.19
In 2015, a study analysed the results of two trials, the dal-OUTCOME and MIRACL, to predict long and short term effects of fasting TGs on recurrent ischemic evens in acute coronary syndrome (ACS) patients already on statins. Results indicated that high TG levels (>175 mg/dL on long term and >195 mg/dL on short term) in spite of statin therapy in postacute coronary artery syndrome (ACS) patients led to an increased CVD risk (60% and 50% higher on long and short term respectively) compared to those patients who had lower TG levels (≤80 mg/dL on long term and ≤135 mg/dL on short term). This relationship of triglycerides to CVD risk was independent of LDL in both studies.20 Wong N et al. classified 4,986 adults (presenting 113 Million population) from USA by fasting TG and estimated 10 years atherosclerotic cardiovascular disease (ASCVD) score based on statin therapy were taken or not. Study concluded that overall 1/4th adults were having high TG (>150 mg/dL), while 14% adults TG was >200 mg/dL. 10-years ASCVD risk score was increasing as TG level was also increasing. It was 10.4% and 16.1% with TG level 200-499 mg/dL and >500 mg/dL, respectively.21
In a recently published study, increased residual CV risk in patients with diabetes and high TG (200-499 mg/dL) despite statin-controlled LDL cholesterol (<100 mg/dL) was observed compared to normal TG level (<150 mg/dL).22 An study of around 28,000 high risk DM patients with TG (200-499 mg/dL) treated with high dose of statin and controlled LDL, showed incidence rate for non-fatal MI was 30% higher, while rate was 23% higher for non-fatal stroke and 21% higher for coronary revascularization compared to normal TG level patients
Elevated triglyceride level is independently associated with increased all-cause mortality in patients with established CHD.23 In a 22 year follow-up, the Bezafibrate Infarction Prevention (BIP) study showed that as TG level is increased from 150 mg/dL to >500 mg/dL, all-cause mortality was also proportionately increasing from 6-68% compared to TG <100 mg/ dL (Figure 3).
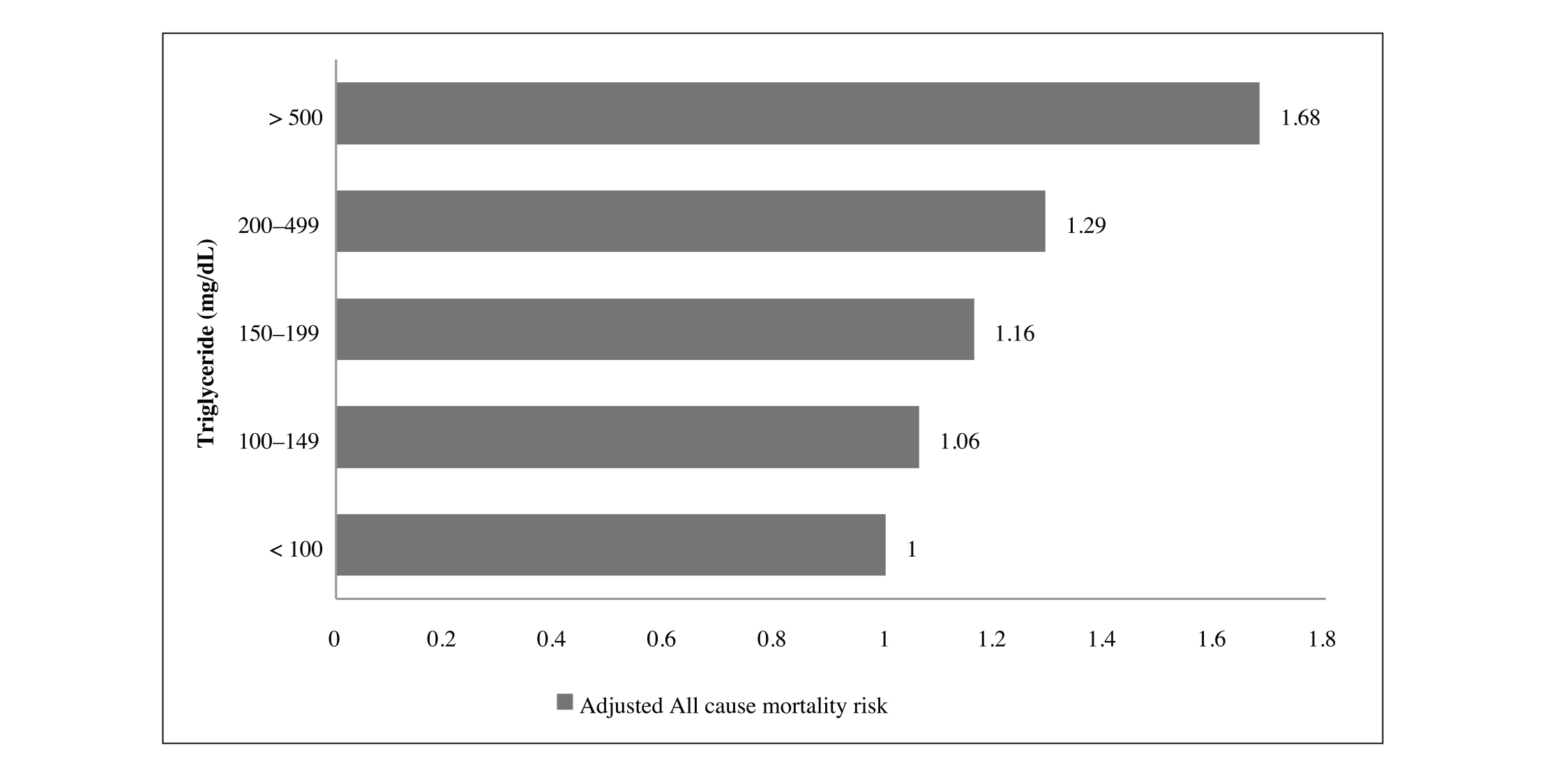
Figure 3. Adjusted all-cause mortality risk according to TG group (22-year follow up BIP- study and registry)23
Fibrates Reduces CV Risk in Patients with TG (>200 mg/dL) with Low HDL (<34 mg/dL)
Thus numerous studies have demonstrated an association between high TG level and CV risk. But the impact of TG lowering therapies on CV events is still unclear as no major outcomes trials have been done in patients with moderate to severe hypertriglyceridaemia as these patients were excluded from statin and fibrate outcomes trials.24
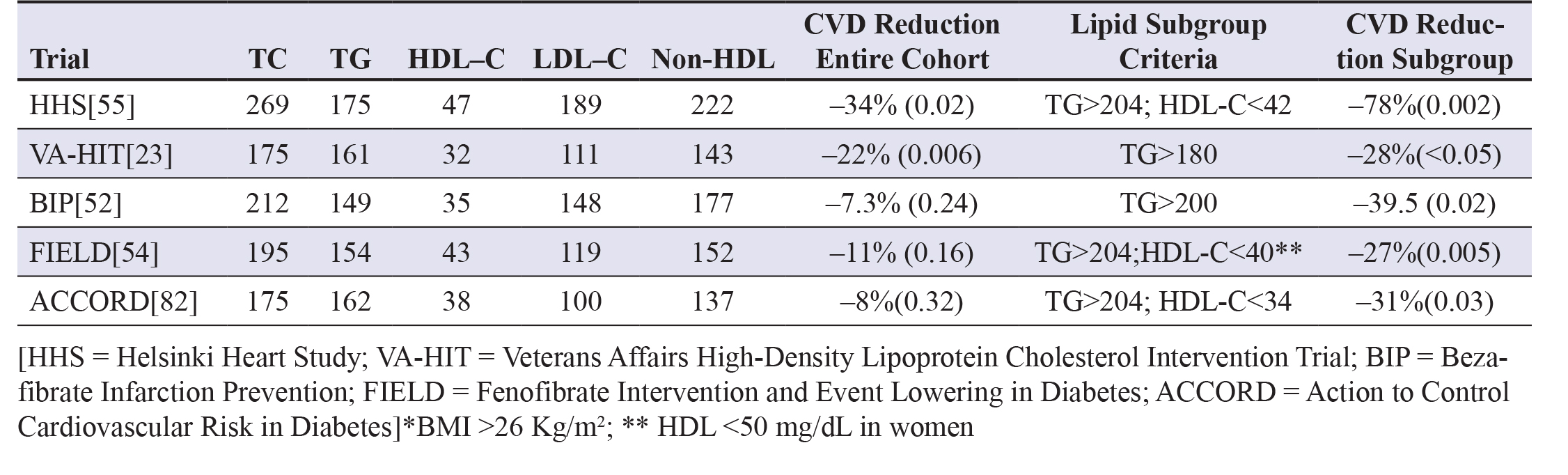
Fibric acid derivatives (fibrates) are predominantly TG lowering agent with modest effect on HDL and least effect on LDL. In general, fibrates are not used in clinical practice to treat individuals with mild hypertriglyceridaemia. As per the Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial (VA-HIT), gemfibrozil has been shown to be effective in both primary and secondary cardiovascular risk reduction in absence of significant change in LDL level (Figure 1).25,26
In contrast, two major trials with fenofibrate in patients with type 2 Diabetes Mellitus have failed to demonstrate reductions in major cardiovascular events (Table 1). The Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study of 9795 diabetic patients with mean levels of TG 154mg/dL, HDL 43 mg/dL, with follow-up over a 5-year study period, failed to demonstrate a significant reduction for CV risk between study groups. But FIELD supported potential safety of combination therapy (fibrate + statin).27 In addition, post hoc analysis of data from the FIELD study demonstrates that patients with elevated TG (>200 mg/dL) or low HDL (<40 mg/dL in men and <50 mg/dL in women) derived greater CV risk reduction with fenofibrate.28
In another study of the Action to Control Cardiovascular Risk in Diabetes lipid trial (ACCORD Lipid), efficacy and safety of statin and fibrate combination was recently evaluated, where in combination failed to show effects on the primary composite outcome (nonfatal myocardial infarction, nonfatal stroke, or CV death), while trend of increased risk was more toward women as compared to men. Of note, in a prespecified subgroup analysis, there was a trend towards benefit of fenofibrate in patients with TG level of ≥204 mg/dL or HDL of ≤34 mg/dL.29
Fibrates have shown CV events reduction in specific subgroup with high TG and low HDL level. Through that hypothesis, it is established that fibrates are to be used in dyslipidaemia patients with high TG and low HDL.30,31
Table 1. Fibrate Outcome Trials30,31
TG Lowering Agent, Icosapent Ethyl (EPA) Significantly Reduces CV Events
In randomized trials, medications that reduce triglyceride levels such as extended-release niacin and fibrates have not reduced the rates of cardiovascular events when administered in addition to appropriate medical therapy, including statins. Even recent meta-analyses of n-3 fatty acid also have not shown a benefit in patients receiving statin therapy.32 In the Japan EPA Lipid Intervention Study (JELIS), 18,645 Japanese patients with hypercholesterolaemia had shown that low-intensity statin therapy plus 1.8 g of eicosapentaenoic acid (EPA) daily, significantly reduced risk of major coronary events by 19%, compared to group that received statin therapy alone.33 JELIS trial results led design of the Reduction of Cardiovascular Events with Icosapent Ethyl Intervention Trial (REDUCE-IT). It is a phase III, randomized, double blind study of 8,179 patients with established CV disease or DM who had been receiving statin therapy with fasting TG level between 135-499 mg/dL were followed up for 4.9 years. The primary end point was a composite of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, coronary revascularization or unstable angina, significant reduced by 25% by icosapent ethyl compared to placebo, along with significant CV death reduction by 20% in treatment group. Finally, this study has concluded that Among patients with elevated triglyceride levels despite the use of statins, the risk of ischemic events, including cardiovascular death, was significantly lower among those who received 2 g of icosapent ethyl twice daily.32
Guideline Recommendations on TG Lowering Therapy
Recently published guidelines for management of dyslipidaemia by the European Society of Cardiology (ESC), 2019 documented that elevated TG rich lipoprotein increase ASCVD risk, so evaluation of TG is essential while managing dyslipidaemia.6 Even ESC, 2019 has also redefined level of TGs for dyslipidaemia management based on outcome data of REDUCE IT and other studies. In high-risk (or above) patients with TG levels between 135-499 mg/dL, despite statin treatment, TG lowering drugs like n-3 PUFAs and icosapent ethyl (2*2 g/day) should be considered in combination with a statin. And for primary prevention patients who are at LDL goal with TG levels >200 mg/dL, TG lowering agents (like fenofibrate or bezafibrate) may be considered in combination with statins. Considering Indians are more prone to develop high TG, the Lipid Association of India (LAI) published guideline on dyslipidaemia management, which has endorsed that statin is first line therapy when TG >200 mg/dL. It is also mentioned that add on to statin, apart from fibrate, Saroglitazar is also approved drug which is safe and effective in T2DM patients with high TG.42
Hypertriglyceridemia and Other Complications
Apart from cardio vascular disease, high TG is also associated with non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), acute pancreatitis (AP). NAFLD is condition which is commonly associated with Obesity and T2DM, where in high free fatty acid is deposited in liver. The survival rate in patients with NAFLD is lower compared to the general population standardized-mortality ratio due to the risk of cardiovascular disease and hepatocellular carcinoma. NAFLD is associated with metabolic disturbances, including diabetes and hyperlipidaemia, especially hypertriglyceridaemia. In study of 168 NAFLD patients, Tomizawa et al. revealed high TG as a strong predictor of NAFLD (χ2 =9.89, P=0.0017).35 Hypertriglyceridaemia is uncommonly associated with acute pancreatitis (AP). European population studies show AP incidence of 10-19% of patients with severe HTG (>1000 mg/dL).36 In a large population study, adjusted hazard ratio for AP was 3 times higher compared to normal patients. Moreover, as TG level is increased by 100 mg/dL, it increase incidence of AP by 4%.37
TG Reducing Agents
As per international guidelines, for management of dyslipidaemia, statins are always considered as a first line therapy focusing on lowering LDL and non HDL. The AHA/ACC, 2018 recommends statin and lifestyle modifications (Class IIa) when there is severe hypertriglyceridaemia with >500 mg/dL and ASCVD score is more than 7.5% considering secondary factors as well.38 Considering the REDUCE IT study CV mortality benefit data, the ESC, 2019 guidelines has redefined recommendations to manage hypertriglyceridaemia with usage of icosapent ethyl add on to statin in high risk patients at TG level between 135-499 mg/dL (Class IIa). While for primary prevention it is recommended to add fibrates to statin when TG is more than 200 mg/dl (Class IIb).6 Fibrates are considered as second line therapy, which is add on to statin and ezetimibe. Fibrates includes many side effects like gastrointestinal symptoms, increased liver function tests, a reversible rise in creatinine and myositis, drug to drug interactions with statin which restrict its usage on regular basis. Omega 3 fatty acid (EPA) has shown CV mortality benefit in the REDUCE IT study, but its usage also leads to common side effects like gastro intestinal (GI) disturbance, diarrhoea, vomiting, belching, foul smelling, poor adherence, etc.40 Saroglitazar is the first New Chemical Entity (NCE) from India and first in class drug which is approved as a dual PPAR α/γ (peroxisome proliferator-activated receptor) agonist, approved for the management of hypertriglyceridaemia in type 2 DM patients uncontrolled with statin alone in India. In Phase III clinical studies, this molecule has shown significant reduction of TG by 45-46.7% and HbA1c reduction by 0.3% without any significant major adverse events. Currently its trials are under evaluation for future indications like type 2 DM and NAFLD in India and global as well.
Conclusion
Hypertriglyceridaemia (>200mg/dL) is considered as CV risk factor, beyond that it contributes in development of NAFLD/ NASH and acute pancreatitis, which are also life threatening conditions. International guideline also recommends high TG level between 135-499 mg/dL as a CV risk factor and its lowering therapy should be considered along with statin. Currently available drugs have some limitation to be used as TG lowering drug. Saroglitazar is effective and safe option as a TG lowering agent for T2DM patients and in future it can be used in more indications like T2DM and NAFLD as well. Saroglitazar has not yet shown its benefit in CV events reduction.
Declaration of conflicting interests
The Authors Declare no Conflict of Interest.
Funding
No funds were received for conducting the study.
References
- INTERHEART Study Investigators; Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with MI in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364:937-52.
- Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014; 384 (9943):626-635.
- Miller M. Dyslipidemia and cardiovascular risk: the importance of early prevention. QJM. 2009; 102(9):657-667.
- Pullinger CR, Aouizerat BE, Movsesyan I, Durlach V, Sijbrands EJ, Nakajima K, et al. An apolipoprotein A-V gene SNP is associated with marked hypertriglyceridemia among Asian-American patients. J Lipid Res. 2008; 49(8):1846-1854.
- Qi X, Hou Y, Guo X. Severe fatty liver disease and acute pancreatitis: is there a correlation between them? Clin Exp Hepatol. 2015; 1(4):127-130.
- Mach F, Baigant C, Catapano A, Koskinas K, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41(1):111-188.
- Gupta R, Rao S, Mishra A, Sharma S. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J. 2017; 69(3):382- 392.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001; 285(19):2486-497.
- Gupta R, Guptha S, Agrawal A, Kaul V, Gaur K, Gupta VP. Secular trends in cholesterol lipoproteins and triglycerides and prevalence of dyslipidemias in an urban Indian population Lipids Health Dis. 2008; 7:40.
- Joshi S, Anjana R, Deepa M, Pradeepa R, Bhansali A, Joshi P, et al. Prevalence of Dyslipidemia in Urban and Rural India: The ICMR–INDIAB Study. PLoS One. 2014; 9(5): e96808.
- Roopa M, Deepa M, Indulekha K, Mohan V. Prevalence of sleep abnormalities and their association with metabolic syndrome among Asian Indians: Chennai Urban Rural Epidemiology Study (CURES-67). J Diabetes Sci Technol. 2010; 4:1524-531.
- Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366(9493):1267- 278.
- Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994; 344:1383-1389.
- Cholesterol Treatment Trialists’ (CTT) Collaborators, Kearney PM, Blackwell L, Collins R, Keech A, Simes J, et al. Efficacy of cholesterol lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: A meta-analysis. Lancet. 2008; 371:117-25.
- Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001; 25:1722-729.
- Tai ES, Emmanuel SC, Chew SK, Tan BY, Tan CE. Isolated low HDL cholesterol: an insulin-resistant state only in the presence of fasting hypertriglyceridemia. Diabetes. 1999; 48:1088-092.
- Miller M. Is hypertriglyceridemia an independent risk factor for coronary heart disease? The epidemiological evidence. Eur Heart J. 1998; 19 (Suppl H):H18-22
- Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E; PROVE IT-TIMI 22 Investigators. Impact of Triglyceride Levels Beyond Low-Density Lipoprotein Cholesterol After Acute Coronary Syndrome in the PROVE IT-TIMI 22 Trial. J Am Coll Cardiol. 2008; 51(7):724-30.
- Schwartz GG, Abt M, Bao W, DeMicco D, Kallend D, Miller M, et al. Fasting Triglycerides Predict Recurrent Ischemic Events in Patients With Acute Coronary Syndrome Treated With Statins. J Am Coll Cardiol. 2015; 65(21):2267-275.
- Wang ND, Fan W, Phillip S, Granowitz C, Toth P. Burden of atherosclerotic cardiovascular disease risk in persons with elevated Triglyceride levels according to statin use. J Am Coll Cardiol. 2019; 73 (9).
- Nichols G, Phillip S, Reynolds K, Fazio S, Granowitz C. Increased residual cardiovascular risk in patients with diabetes and high versus normal triglycerides despite statin-controlled LDL cholesterol. Diabetes Obes Metab. 2019; 21:366-371.
- Klempfner R, Erez A, Sagit B, Goldenberg I, Fisman E, Kopel E, et al. Elevated Triglyceride Level Is Independently Associated With Increased All-Cause Mortality in Patients With Established Coronary Heart Disease Twenty-Two–Year Follow-Up of the Bezafibrate Infarction Prevention Study and Registry. Circ Cardiovasc Qual Outcomes. 2016; 9(2):100-08.
- Sampson U, Fazio S, Linton M. Residual Cardiovascular Risk Despite Optimal LDL-Cholesterol Reduction with Statins: The Evidence, Etiology, and Therapeutic Challenges Curr Atheroscler Rep. 2012; 14(1):1-10.
- Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs High Density Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med. 1999; 341:410-418
- Manninen V, Elo MO, Frick MH, Haapa K, Heinonen OP, Heinsalmi P, et al. Lipid alterations and decline in the incidence of coronary heart disease in the Helsinki Heart Study. JAMA. 1988; 260:641-651.
- Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005; 366:1849- 1861.
- Sacks FM. After the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study: implications for fenofibrate. Am J Cardiol. 2008; 102:34L-40L
- ACCORD Study Group, Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1563-1574.
- Barter PJ, Rye KA. Is there a role for fibrates in the management of dyslipidemia in the metabolic syndrome? Arterioscler Thromb Vasc Biol. 2008; 28:39-46.
- Elam M, Lovato LC, Ginsberg H. Role of fibrates in cardiovascular disease prevention, the ACCORD-Lipid perspective. Curr Opin Lipidol. 2011; 22:55-61.
- Bhatt D, Stag G, Miller M, Brinton E, Jacobson T, Ketchmun S, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019; 380:11-22
- Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomized open-label, blinded endpoint analysis. Lancet. 2007; 369:1090-098.
- Bhatt DL, Steg PG, Brinton EA, Jacobson TA, Miller M, Tardif JC, et al. Rationale and design of REDUCE-IT: Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial. Clin Cardiol 2017; 40: 138-48.
- Tomizawa M, Kawanabe Y, Shinozaki F, Sato S, Motoyoshi Y, Sugiyama T, et al. Triglyceride is strongly associated with nonalcoholic fatty liver disease among markers of hyperlipidemia and diabetes. Biomed Rep. 2014; 2(5):633-636.
- Valdivielso P, Ramirez-Bueno A, Ewald N. Current knowledge of hypertriglyceridemic pancreatitis. Eur J Intern Med. 2014; 25(8):689-94.
- Murphy MJ, Sheng X, Macdonald TM, Wei L. Hypertriglyceridemia and acute pancreatitis. JAMA Intern Med. 2013; 173(2):162-64.
- Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 73(24):3168-3209.
- Remick J, Weintraub H, Setton R, Offenbacher J, Fisher E, Schwartzbard A. Fibrate therapy: an update. Cardiol Rev. 2008; 16(3):129-41.
- Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, et al. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease A Science Advisory From the American Heart Association. Circulation. 2017; 135:e867-e884.
- Shetty SR, Kumar S, Mathur RP, Sharma KH, Jaiswal AD. Observational study to evaluate the safety and efficacy of saroglitazar in Indian diabetic dyslipidemia patients. Indian Heart J. 2015; 67(1):23-6.
- Iyengar SS, Puri R, Narasingan SN, Wangnoo SK, Mohan V5, Mohan JC, et al. Lipid Association of India Expert Consensus Statement on Management of Dyslipidemia in Indians 2016: Part 1. J Assoc Physicians India. 2016; 64(3 suppl):7-52.
